Denosumab could half number of redo hip replacement operations
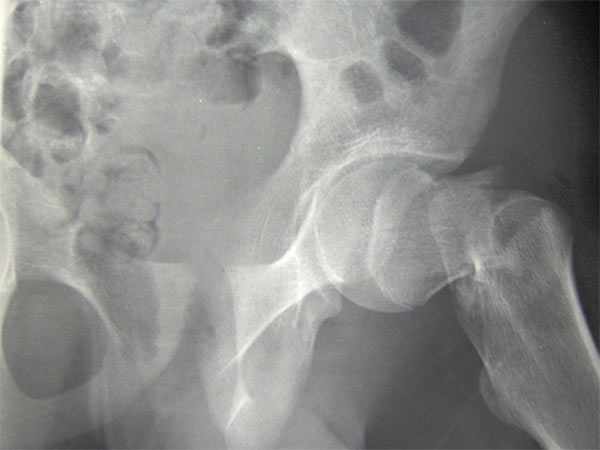
Osteolysis – a disease that eats away at bone tissue – is the leading reason for joint replacement reoperation
An estimated 8,500 hip revision procedures are conducted in England, Wales and Northern Ireland each year at a large cost to the NHS, with repeat procedures less likely to be as effective as first time surgery due to weakened bone.
Researchers from the University of Sheffield found the osteoporosis drug, denosumab, could protect patients from osteolysis, reduce the need for re-operations, and reduce the health burden of this disease
More than half of repeat hip replacement operations could be prevented with a drug already successfully used to treat osteoporosis, new research from the University of Sheffield and Sheffield Teaching Hospitals NHS Foundation Trust has revealed.
An estimated 8,500 hip revision procedures are conducted in England, Wales and Northern Ireland each year at a large cost to the NHS, with repeat procedures also carrying an increased risk of infection and other complications compared to first time surgery.
The leading reason for joint reoperation is osteolysis – a disease that eats away at bone tissue causing it to weaken and dissolve. The disease occurs after joint replacement surgery when tiny particles wear off from the implant causing the body’s immune system to attack the already weakened bone around the implant. This causes the artificial joint to loosen, causing pain and eventually requiring revision surgery.
The pioneering study, led by Professor Mark Wilkinson from the University of Sheffield’s Department of Oncology and Metabolism in partnership with Sheffield Teaching Hospitals NHS Foundation Trust, found a drug already used to treat osteoporosis, called denosumab, could help to protect the bone from being attacked and prevent the need for some repeat hip replacement operations.
“For decades scientists have been looking for a therapy that will help to protect vulnerable areas of bone and prevent revision surgery which not only has huge cost implications for the NHS, but also causes pain and reduces mobility for patients,” said Professor Wilkinson.
“This study is a significant breakthrough as we’ve demonstrated there is a drug, already available and successful in the treatment of osteoporosis, which has the potential to prevent up to half of all revised replacement surgeries which are caused by osteolysis.
“A primary hip replacement costs around £6,000. However, revision replacements can cost the NHS three times as much at approximately £18,000. Revision surgery is an extensive procedure and carries much higher risks of infection and other complications compared to first time surgery, and the recovery period is longer and more painful.”
He added: “Using the antibody therapy denosumab to prevent the need for a second hip replacement could have a huge impact on thousands of patients who currently undergo revision surgery every year. This is particularly good news for younger patients and those with higher activity levels who tend to wear away the plastic part of the implant quicker.”
The findings, published in the journal The Lancet Rheumatology, show that the treatment kills around 90 per cent of the cells responsible for bone loss in patients due to have revision hip surgery who were treated with denosumab. A total of 22 patients took part in the Phase 2 clinical trial sponsored by Sheffield Teaching Hospitals and funded by Amgen, Inc.
Professor Wilkinson, who is an Honorary Consultant Orthopaedic Surgeon at Sheffield Teaching Hospitals Foundation Trust, said: “It is very clear from our bone biopsies and bone imaging that the injection stops the bone absorbing the micro-plastic particles from the replacement joint and therefore could prevent the bone from being eaten away and the need for revision surgery.
“We are now hoping to conduct a much bigger Phase 3 clinical trial and are seeking opportunities to continue this ground breaking research which could revolutionise how we treat patients found to be at risk of needing a secondary joint replacement.”
Edward Whittle, 80, from Sheffield had two revision hip operations due to osteolysis, believes the study’s findings could make a difference to patients like him in the future.
“I had my first hip replacement around 10 years ago, however the second replacement surgery was a lot different to the first one and it took me a lot longer to get back on my feet,” said Edward.
“I was in a great deal of pain for around 12 months and I took a lot of looking after.
“I think it would be absolutely fantastic if a simple injection could help to prevent people from having to undergo repeat replacements – it would be so much better for patients and their families.
“If this treatment was available after my first replacement it would have made such a big difference to me.”
The research was conducted in collaboration with Sheffield Teaching Hospitals NHS Foundation Trust who sponsored the study and used their significant medical expertise to report on the cells and tissue samples.
David Hughes, Medical Director (Development) for Sheffield Teaching Hospitals NHS Foundation Trust, who was involved in the study, said: “We are delighted to have contributed to this important study demonstrating the effectiveness of a treatment against osteolysis in clinical trials for the very first time. Larger scale trials are required to show that the need for future surgery can be reduced, but these initial results are hugely encouraging.”
Professor Wilkinson and his team are now hoping to develop the research into a Phase 3 trial to further assess the clinical effectiveness of the novel treatment.
Source: Sheffield, University of
Full bibliographic information
The Lancet Rheumatology
Effect of denosumab on osteolytic lesion activity after total hip arthroplasty: a single-centre, randomised, double-blind, placebo-controlled, proof of concept trial