Preventive Percutaneous Coronary Intervention for High-Risk Coronary Plaques Reduces Cardiac Events
PCI shows substantial benefits over medications alone
People with a buildup of fatty atherosclerotic plaque in the heart’s arteries considered at risk of rupturing were far less likely to suffer a serious cardiac event if they underwent percutaneous coronary intervention (PCI), a procedure to open blocked arteries, compared with those who took medications alone but did not undergo PCI, according to research presented at the American College of Cardiology’s Annual Scientific Session.
PCI is commonly used to open blocked arteries to treat significant myocardial ischemia, which occurs when the heart muscle does not get enough oxygenated blood. These new findings suggest that people with high-risk plaques that are likely to rupture could benefit from the procedure as a pre-emptive measure rather than waiting for a heart attack or other severe reduction in blood flow to occur.
The PREVENT trial is the largest study on preventive PCI to date—meaning it involves patients whose blockages were not severe enough to cause symptoms or ischemia and would not otherwise undergo PCI according to current standard of care—and the first with a large enough sample size to assess clinical outcomes of its use in treating vulnerable plaques. At two years, people who underwent preventive PCI were 89% less likely to experience the composite primary endpoint of cardiac death, heart attack in the target vessel, revascularization due to ischemia in the target vessel or hospitalization for unstable or progressive chest pain compared with people who received medications alone.
“PREVENT has now shown that preventive PCI may reduce the two-year and long-term risks of major cardiac events arising from vessels containing vulnerable plaques,” said Seung-Jung Park, MD, professor in the Division of Cardiology at Asan Medical Center at the University of Ulsan College of Medicine in Seoul, South Korea, and the study’s lead author. “These findings demonstrate that the focal treatment of high-risk vulnerable plaques may improve patient prognosis beyond optimal medical therapy alone.”
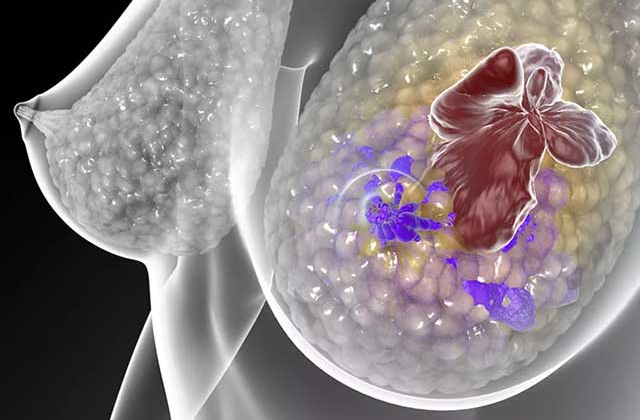
Plaques that build up in the heart’s arteries contain fats, cholesterol and other substances; most heart attacks and serious cardiac events occur when pieces of such plaques break off and travel through the blood vessel, causing a blockage. During PCI, an operator inserts a stent into a blocked artery through a catheter in the groin or arm. The stent is left in place, where it props the artery open to allow blood to flow freely; medications eluted by the stent can also help to prevent further plaque buildup.
The idea behind preventive PCI is that a stent could help to stabilize a high-risk plaque lesion and thus reduce its risk of rupture before a heart attack occurs. To test this strategy, researchers enrolled 1,606 patients treated for coronary artery disease at 15 centers in four countries. All participants had plaques that were considered vulnerable to rupture, as assessed with intravascular imaging, but were not limiting blood flow through the artery, as indicated by a fractional flow reserve greater than 0.80. Patients were 64 years old, on average.
Half of the participants were randomly assigned to receive PCI plus medical therapy and half received medical therapy alone. Optimal medical therapy for coronary artery disease includes lifestyle modifications and intensive pharmacologic interventions, according to the contemporary guideline-directed medical therapy for secondary prevention. High-dose statin therapy was strongly recommended in both groups.
At two years, the composite primary endpoint occurred in three patients who received PCI (0.4% of the PCI group) and in 27 patients who received medications alone (3.4% of the controls), representing an 89% lower risk of the composite primary endpoint among those who received PCI. The cumulative incidence of this composite endpoint remained significantly lower in the PCI group through long-term follow-up over a median of 4.4 years (maximum up to 7.9 years), with patients receiving PCI showing a 46% lower risk of the composite endpoint across this period.
Rates for each component of the composite primary endpoint were also lower in the PCI group, as were the composite rate of death from any cause or heart attack in the target vessel or any revascularization.
Since study participants and their clinicians were aware of which treatment patients were assigned to receive, the lack of blinding could have introduced bias and influenced the study results, researchers said. Park added that the study was limited to patients with non-flow-limiting plaques that were detected with intravascular imaging and is not necessarily generalizable beyond this patient population. The study also was geographically limited to East Asia and nearly three-quarters of the participants were men.
“Further research is necessary to provide better identification of which patients or lesions can most benefit from invasive or non-invasive imaging evaluation for detection of vulnerable plaques, optimal risk-stratification and the application of preventive PCI,” Park said.
Researchers also said that the observed rates of the primary outcome were lower than expected in both groups. This could be related to a combination of factors, including the relatively low proportion of study participants with acute coronary syndromes; improvements in medical therapy and in PCI equipment and techniques, including the use of intravascular imaging-guided PCI; and effective control of risk factors such as low-density lipoprotein (LDL) cholesterol.
The study was funded by Cardiovascular Research Foundation, Abbott, Yuhan Corp, CAH-Cordis, Philips and Infraredx, a Nipro company.
This study was simultaneously published online in The Lancet at the time of presentation.
Park will be available to the media in a press conference on Monday, April 8, 2024, at 12:30 p.m. ET / 16:30 UTC in Room B203.
Park will present the study, “Preventive PCI or Medical Therapy Alone for Atherosclerotic Coronary Vulnerable Plaques,” on Monday, April 8, 2024, at 11:00 a.m. ET / 15:00 UTC in the Hall B-1 Main Tent.
ACC.24 will take place April 6-8, 2024, in Atlanta, bringing together cardiologists and cardiovascular specialists from around the world to share the newest discoveries in treatment and prevention. Follow @ACCinTouch, @ACCMediaCenter and #ACC24 for the latest news from the meeting.
The American College of Cardiology (ACC) is the global leader in transforming cardiovascular care and improving heart health for all. As the preeminent source of professional medical education for the entire cardiovascular care team since 1949, ACC credentials cardiovascular professionals in over 140 countries who meet stringent qualifications and leads in the formation of health policy, standards and guidelines. Through its world-renowned family of JACC Journals, NCDR registries, ACC Accreditation Services, global network of Member Sections, CardioSmart patient resources and more, the College is committed to ensuring a world where science, knowledge and innovation optimize patient care and outcomes. Learn more at ACC.org.
Full bibliographic information
Published on 08/04/2024 by American College of Cardiology
This study was simultaneously published online in The Lancet at the time of presentation.