The new ‘alternative’ for menopause
| Moira Mizzi |
Plants have formed an integral part of our existence since time immemorial and since then we have been using them in many forms to support our survival. The use of plants or plant extracts for medicinal purposes has also been extensively explored and the intricacy of this research has followed the vertiginous progress in diagnostics and intervention. The use of synthetic chemicals for the cure of disease has nowadays taken up much of the pharmaceutical field; despite this, herbalism, or the study and use of plants as medicinals, is still a thriving facet of the pharma industry.
One of the medical fields in which herbalism is trying to establish a valid market is gynaecology, more specifically the menopause. Menopause is a highly particular phase in a woman’s life that marks the end of fertility and slowly but determinedly steers her into middle and old age. It is a time of great physiological and psychological change which, if not tackled well, could lead to deleterious repercussions in both aspects. The hallmark of this biological havoc is a progressive decrease in the production of oestrogen by the ovaries which, if not corrected, could result in day-to-day inconveniences such as hot flushes, vaginal dryness, sleeping problems and mood swings to more serious consequences like osteoporosis and cardiovascular disease.
Replacing the depleted oestrogen is a natural solution to this predicament. For many decades, in fact, the rationale of the treatment for menopausal symptoms has hinged around oestrogen replacement, what is more commonly described as HRT or hormone replacement therapy, in the form of oral tablets, slow release subcutaneous administrations or local creams for vaginal dryness. Although their efficacy is close to optimal, even where the irritating day-to-day symptoms are concerned, the adverse events they can create can be quite hazardous especially where heart disease and breast cancer in susceptible individuals are concerned.
Complementary alternative medicines or CAMs have been a popular alternative or additive1, especially in the United States2,3, where at least 40% of the population uses a CAM at any one time or the other, with women over the age of 40 being the most avid users4. The publication of the results of the Women’s Health Initiative randomised controlled trial in 20025, which highlighted a negative benefit-risk ratio with the prolonged use (5.2 years) of hormone therapy in older postmenopausal women also shifted the onus of popularity on the ‘alternatives’. The CAMs most commonly used are herbal remedies and dietary phytoestrogens.
Herbal remedies come in various forms, including black cohosh, dong quai, ginseng, red clover and evening primrose oil. The most popular and the most studied herb is black cohosh whose medicinal use in gynaecology dates back to the Native Americans. Some clinical studies have found it effective in the treatment of hot flushes; however none of these trials have lasted more than six months and thus its efficacy in the long term is questionable2. Other clinical trials found no benefits when compared to placebo and in one trial6, black cohosh appeared to be mostly effective in a subset of women with recent onset of menopause3.
The identity of the active compounds of black cohosh are still unknown, and this presents an uncertainty both about its mode of action and its safety profile. Sadly, this is the dilemma faced with a number of herbal remedies launched on the market. The fact that most of the clinical trials are not placebo-controlled and only span a short period of time does nothing to help the situation2.
Dietary phytoestrogens, extracted from a variety of food plants such as soy, beans and clover, are another alternative in the natural remedy repertoire. Interest in these products was sparked when high dietary intakes of soy was postulated to be one of the reasons of low incidence of menopausal symptoms in Japan, China and Korea. Composed of phenolic (rather than steroidal) compounds, these substances include chemicals such as isoflavones which when acted on by intestinal bacteria are converted from the conjugated to the unconjugated active forms such as genistein, daidzein and equol2.
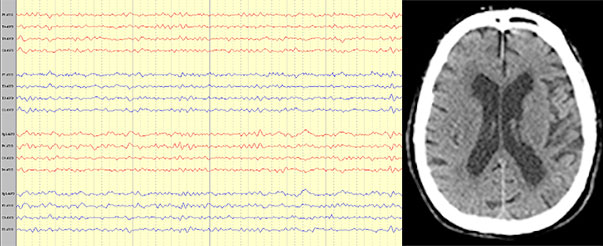
The mode of action of the isoflavones is clearer than their herbal counterparts. The oestrogen receptor is particular amongst the other steroid receptors in that it has the ability to bind with a wide range of molecules. It is made up of an α and a β counterpart – the α part of the receptor is responsible for breast and uterus while the β aspect controls bone, blood vessels and the brain (diagram 1). The 17-β oestradiol molecule found in hormone replacement therapy is non-selective and this in fact results in the deleterious cardiac, uterine or breast side effects in susceptible individuals. Isoflavones, on the other hand have more affinity for the β-part of the receptor and thus is more selective to vasomotor, psychological and osteoporotic symptomatology7.
Despite their promising mode of action, the niche for the isoflavone market seems to focus mostly on the vasomotor symptoms of menopause. 11 clinical trials have examined the use of isoflavones for hot flushes2; of these, only 3 out of 8 studies lasted more than 6 weeks and no particular efficacy was found even when used in moderately long term (24 weeks). Comparisons were not possible due to the different product, dosage and scoring systems used and the same beneficial effects were found both in the study and the placebo groups2. On the other hand, recent placebo-controlled double-blind studies showed promising results8, and a 2012 systematic review and meta-analysis of randomized controlled trials concluded that soy isoflavone supplements are significantly more effective than placebo in the reduction of hot flashes.9
Omega-3-fatty acids have also been considered as a treatment for hot flushes and psychological distress, especially considering their recommendable safety profile and known beneficial cardiovascular effects3. Even if studies so far, have been encouraging10, their role in menopausal women without overt psychological symptoms is still unknown.
Considering their popularity and widespread use, it is clear that despite their hazy clinical profile, complementary alternative medicines have found their place in the menopause community. I believe that better planned clinical trials with a larger number of participants and taking place over more extended timelines could yield more scientifically coherent data which would certainly support more their acceptance in the clinical scenario. After all, complementary, alternative or otherwise, harmonisation and standardisation of marketing protocols for all medicinals is the best way forward to transparency and accountability in the pharma industry.
References
1. Speroff L. Alternative Therapies for Postmenopausal Women. Int J Fertil Womens Med. 2005; 50(3): 101-14.
2. Kronenberg F et al. Complementary and Alternative Medicine for Menopausal Symptoms: A Review of Randomised, Controlled Trials: Ann Intern Med. 2002; 137: 805-813.
3. Pasciullo, BA&Joffe, MD, MSc. Use of Complementary and Alternative Medicines for Menopausal Hot Flashes. Massachusetts Centre for Women’s Health: May 29, 2009.
4. Barnes PM, et al. CDC National Health Statistics Report #12. Complementary and Alternative Medicine Use Among Adults and Children: United States, 2007. December 10, 2008.
5. Roussouw JE et al. Risks and benefits of oestrogen plus progestin in healthy postmenopausal women: principal results from the Women’s Health Initiative randomised controlled trial. JAMA 2002: 288(3) 321-33.
6. Osmers R et al. Efficacy and safety of isopropanolic black cohosh extract for climacteric symptoms. Obstet Gynaecol 2005: 105(5) 1074-83.
7. Kuiper et al. Interaction of Estrogenic Chemicals and Phytoestrogens with Estrogen Receptor β. Endocrinology 139 (10): 4252-63.
8. Imhof M et al. Improvement of menopausal symptoms by soy isoflavones: a randomized double-blind study Planta Med 2008; 74 – SL86.
9. Taku K et al. Extracted or synthesized soybean isoflavones reduce menopausal hot flash frequency and severity: systematic review and meta-analysis of randomized controlled trials. Menopause. 2012 Jul;19(7):776-90.