Ultrasound Assessment of right upper quadrant abdominal pain – Part 1
kAuthor : Dr Pierre Vassallo
Right Upper Quadrant (RUQ) abdominal pain is one of the most common presenting complaints to any clinic or emergency department. Acute cholecystitis is the most frequent cause, however more than a third of cases are due to other conditions.
Due to the numerous possible aetiologies of RUQ abdominal pain, a rapid test for identifying the cause and guiding further detailed investigation is required. Abdominal ultrasound (US) is the imaging modality of choice as a first investigation;1 it is readily available, rapid, cost-effective, and safe since it involves no ionising radiation or potentially nephrotoxic intravenous contrast agent. Abdominal US also assesses multiple upper abdominal organ systems that could be the source of the patient’s pain. It readily distinguishes other causes of pain including hepatic, pancreatic, adrenal, renal, vascular, intestinal and thoracic causes. Biliary and hepatic causes of RUQ pain will be discussed in this article. Discussion of other causes will appear in a follow-up article.
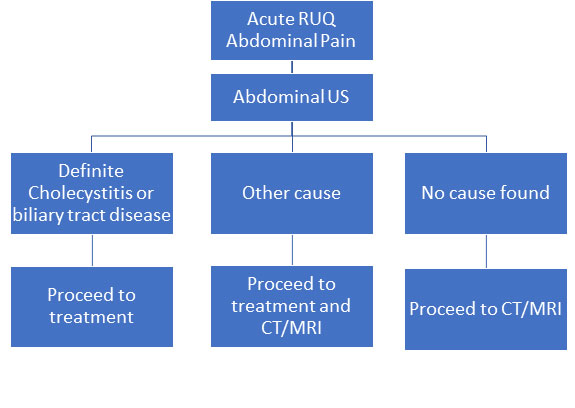
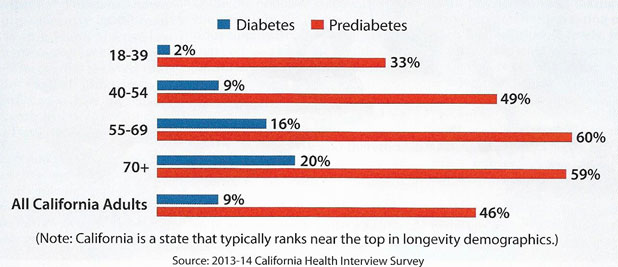
Figure 1 below shows the recommended algorithm for investigating RUQ abdominal pain.2
Acute cholecystitis presents with RUQ abdominal pain that may radiate to the right shoulder and may be accompanied by nausea, vomiting, and fever. Tenderness under the right costal margin sometimes with a positive Murphy’s sign (accentuation of pain during inspiration) are the classical presenting signs, however they are not pathognomonic. Confirmation of clinically suspected cholecystitis, assessment of its severity and exclusion of alternative causes with US are needed.
Ninety to 95% of cases of acute cholecystitis are due to gall stones (calculous cholecystitis). On US, gall stones may be seen (Figure 2a) to obstruct the gall bladder neck or cystic duct. A positive sonographic Murphy’s sign, whereby pain is accentuated during inspiration while the examining probe applies pressure on the gall bladder, helps to confirm the diagnosis. Gall bladder wall thickening (Figure 2b), sludge in the gall bladder and fluid outside the gall bladder are all features of acute cholecystitis. Gas bubbles in the gall bladder wall seen on ultrasound are indicative of gangrenous cholecystitis and represent a surgical emergency.
Hepatic causes of RUQ abdominal pain usually relate to any pathological process that distends the liver capsule; these processes may include hepatitis, hepatic enlargement due to steatosis, liver abscesses and liver neoplasms with or without intra-tumoural haemorrhage.
Hepatitis refers to any form of inflammation of the liver, which may be due to viral infection, medications, drugs, toxins, alcohol or autoimmune disease. It leads to enlargement of the liver, which presents on ultrasound as a cranio-caudal diameter of the liver over 15.5cm at the mid-clavicular line. An anterior liver margin extending below the lower pole of the right kidney is also indicative of an enlarged liver. A heterogeneous hypoechoic parenchymal texture in an enlarged liver (Figure 3a) is suggestive of hepatitis. Hyperechoic thickening around the main portal structures (Figure 3b) may be evident in acute hepatitis and is due to oedema (and consequently hypoechogenicity) of the background liver parenchyma. Numerous thickened portal triads distributed throughout the oedematous liver have been referred to a “starry night appearance” (Figure 3c). Finally, acute hepatitis may result in reactive oedema of the gall bladder wall (Figure 3d) with gall bladder wall thickening in the absence of stones or sludge. Computed tomography (CT) and magnetic resonance imaging (MR) may be used in equivocal cases and may show hepatomegaly, periportal oedema and periportal lymphadenopathy (Figure 3e).
Steatosis hepatis (or fatty liver) refers to an increased level of intracellular fat within hepatocytes. It may present in two forms: focal or diffuse. Both forms appear to have the same aetiology; they are more common in diabetic and obese patients, in cases of alcohol abuse or overeating and in association with drug use (exogenous steroids, amiodarone, methotrexate and chemotherapeutic agents). The steatotic portion of the liver will exhibit increased echogenicity on ultrasound, low density on CT and increased signal on T1-weighted MR images. Detection of the altered texture may be facilitated by comparison with the renal parenchyma on ultrasound (fatty liver has higher echogenicity) (Figure 4) and the spleen on CT and MR (fatty liver has lower density on CT and higher signal on T1-weighted images). MR imaging using various fat suppression techniques and intravenous contrast injection is highly useful in confirming the diagnosis.
Hepatic abscesses are uncommon, but they do present with RUQ abdominal pain. Infection may enter through the portal vein (from e.g. diverticulitis, appendicitis), the hepatic artery (e.g. endocarditis or septicaemia) or the biliary tree (e.g. ascending cholangitis); in these cases, multiple hepatic abscesses may be present. Rarely infection may enter the liver from the right lung or through penetrating injury. Hepatic abscesses present with RUQ abdominal pain and fever. Blood cultures are only positive in 50% of cases. Infections may be pyogenic, fungal or mixed, sometimes parasitic (entamoeba or echinococcus). Liver abscesses are more common in immuno-deficient states. US depicts liver abscesses as hypoechoic thick-walled lesions with indistinct margins and thick septa (Figure 5a); hyperechoic areas within the lesions correlate with debris and gas. Colour Doppler US shows peripheral vascularity of the lesion. In some cases, further imaging is required to distinguish these lesions from necrotic tumours. CT depicts abscesses as hypodense with thick irregular contrast-enhancing rims; the appearance of a cluster of ring-enhancing lesions has been called the cluster sign and is strongly suggestive of an abscess (Figure 5b).
Hepatic tumours may present with RUQ abdominal pain. Since pain is mainly the result of capsular distension, small tumours rarely cause pain. Rapidly-growing tumours or smaller tumours with secondary intra-tumoural haemorrhage may present with pain. Hepatocellular adenomas (“hepatic adenomas”), hepatocellular carcinomas, large haemangiomas, peliosis and metastases may all develop intra-tumoural haemorrhage; this is rare in focal nodular hyperplasia. Pain is particularly evident if the expanding lesion has a subcapsular location. Hepatic adenomas are normally hyperechoic because they contain fat; secondary haemorrhage would appear as hypoechoic or anechoic areas within the lesion (Figure 6a) and peritoneal free fluid may be present if the liver capsule leaks. Hepatocellular carcinomas may have clear or ill-defined margins and may vary from hyper- to hypoechoic depending on their fat content; these differences parallel the aggressiveness (low to high) of the tumour. Haemorrhage into a hepatocellular carcinoma will appear similar to haemorrhage in any other tumour; these lesions are best assessed with CT or MR that help distinguish haemorrhage from viable tumour tissue (Figure 6b). Eighty percent of hepatocellular carcinomas develop in cirrhotic livers.
Other conditions that result in RUQ abdominal pain will be discussed in a follow-up article that will appear in the next issue of The Synapse Journal.
Bibliography
- American College of Radiology. ACR Appropriateness Criteria: right upper quadrant pain. https://acsearch.acr.org/docs/69474/Narrative/. Published 1996. Updated 2013. Last review date: 2013. Accessed January 26, 2018.
2. Joshi G, Crawford KA, Hanna TN et al. US of Right Upper Quadrant Pain in the Emergency Department: Diagnosing beyond Gallbladder and Biliary Disease. Radiographics 2018;38(3):766-793.
Figure Legends
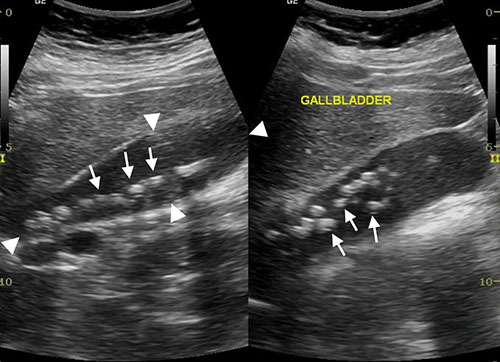
Figure 2a: Longitudinal US scan of the gall bladder containing numerous calculi (arrows).

Figure 2b: Longitudinal US scan of the gall bladder showing thickening of the posterior wall (arrows).
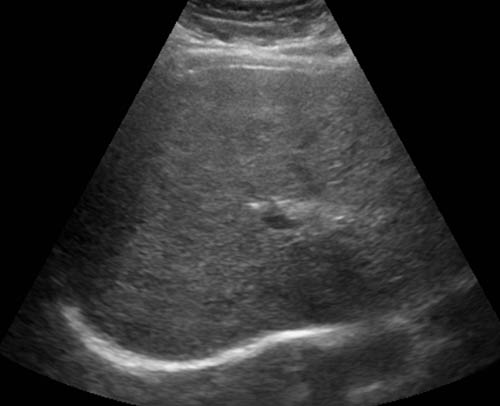
Figure 3a: Transverse US scan of the liver: Heterogeneous hyperechoic liver texture is due to acute hepatitis.

Figure 3b: US scan through the porta hepatis: Hyperechoic thickening around portal structures due to acute hepatitis
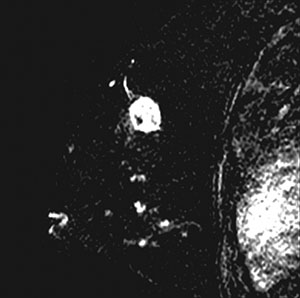
Figure 3c: Transverse US scan through the liver: “Starry sky” appearance due to background liver parenchymal hypoechogenicity resulting in hyperechoic thickening around the portal triads.
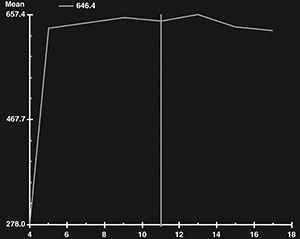
Figure 3d: Longitudinal US scan through the gall bladder: Gall bladder wall thickening secondary to acute hepatitis.
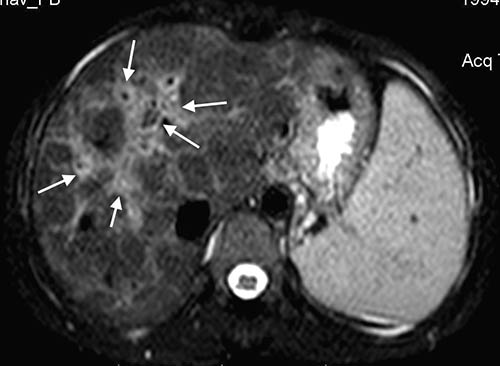
Figure 3e: Transverse T2-weighted MR scan of the liver showing periportal oedema (arrows).
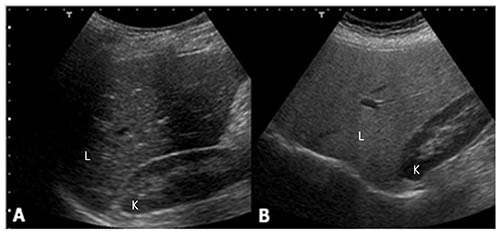
Figure 4: Sagittal US scans through the liver (L) and right kidney (K): note that in the normal case (A) echogenicity of liver and renal parenchyma are similar, while in a fatty liver (B), the liver parenchyma is hyperechoic.
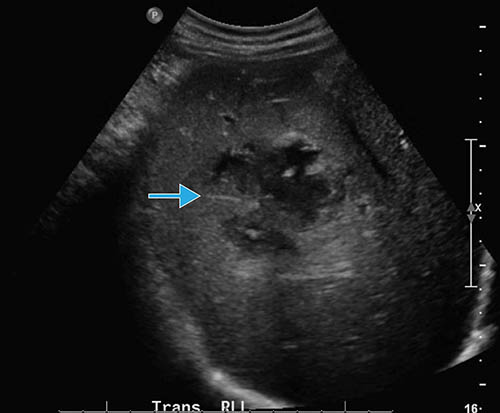
Figure 5a: Transverse US scan through the liver: The liver abscess (arrow) shows partly ill-defined margins with anechoic (fluid-containing) areas.

Figure 5b: Coronal CT Image showing a liver abscess (arrow) with the typical “cluster sign”. Also note surrounding low density that represents oedematous liver parenchyma.

Figure 6a: Transverse US scan through the liver: the hepatocellular adenoma (circle) has ventral isoechoic components and dorsal hyperechoic areas, the latter representing intra-tumoural haemorrhage.

Figure 6b: Transverse contrast-enhanced CT scan through the liver: The enhancing hepatocellular carcinoma (white arrows) is in a subcapsular location. There is peritoneal fluid (*) and peritoneal metastases are present, both indicating capsular leak.