Breast Cancer Imaging: Ductal Carcinoma in-situ (DCIS) – Part II
by Pierre Vassallo
DCIS is rarely seen on US, where it may appear as a microlobulated mass with mild hypoechogenicity, ductal extension, and normal acoustic transmission.
Recent studies conducted at higher spatial resolution MRI have increasingly been performed to screen higher-risk women as well as to evaluate extent of disease. The sensitivity of MR imaging for detection of DCIS has been shown to be higher for high-grade and intermediate-grade DCIS as compared with low-grade DCIS (98%, 91%, and 80%, respectively). Overall, MR imaging is more sensitive than mammography in the detection of all grades of DCIS. Over the past decade, studies have shown that the sensitivity of MRI for DCIS has improved significantly and is much higher than that of mammography (92% vs 56%, respectively).
DCIS most commonly appears on contrast enhanced T1-weighted MRI scans as an area of Non-Mass Enhancement (NME) (Fig 9), which is an area of enhancement without evidence of a mass or focal lesion on non-enhanced scans. DCIS manifests as NME in 60–81% of cases, as a mass in 14–41% of cases or as a focal lesion on non-enhanced scans in 1–12% of cases. Subtraction of pre-contrast from post-contrast enhanced images significantly improves lesion conspicuity. DCIS is usually not visible on non–contrast material–enhanced T1-weighted images or on non–fat-saturated or fat-saturated T2-weighted images because it is masked by the normal breast parenchyma. DCIS may sometimes appear bright on T2-weighted images because of either ductal secretions or necrosis.
DCIS on contrast enhanced T1-w scans may have a linear (Fig 10), segmental (Fig 11) or regional (Fig 12) distribution.
Kinetic assessment of contast enhancement (time/enhancment pattern) is also helpful in distinguishing benign from malignant lesions with breast MRI. A wash-out pattern of contrast enhancment (loss of signal intensity following the uptake phase) is more indicative of a malignant lesion while persistent enhancement is usually seen in benign lesions (Figs 13 and 14).
DCIS may appear nodular or as a mass lesion, and kinetic studies are not always reliable in DCIS (Fig 15). Follow-up examinations may be required for equivocal lesions as a negative biopsy may be due to incorrect sampling. Nodular or mass lesions may have homogeneous, heterogeneous or rim-enhancement patterns; the heterogeneous enhancement patter is most common in DCIS.
The extent of DCIS is often underestimated at mammography because mammography does not usually reveal noncalcified DCIS. MR imaging has been shown to depict more accurately the extent of DCIS because of its ability to demonstrate noncalcified DCIS.
Of all imaging tools available, MR imaging has the highest sensitivity in the detection of DCIS. DCIS has a variety of MR imaging features that need to be recognised.
Figure Legends
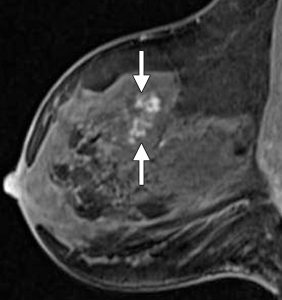
Figure 9. High-grade DCIS in a BRCA2-positive woman appearing as a 2.5-cm area of linear, clumped NME (arrows) on sagittal postcontrast T1-w scans.
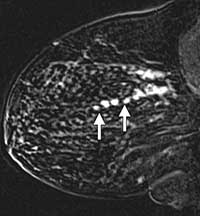
Figure 10. Intermediate-grade DCIS seen on contrast-enhanced T1-w scans as multiple round areas of NME distributed in a linear distribution.
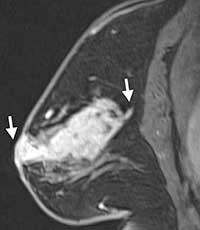
Figure 11. Intermediate-grade DCIS seen on contrast-enhanced T1-w scans as a segmental area of enhancment (arrows).

Figure 12. Intermediate-grade DCIS seen on contrast-enhanced T1-w scans as a regional area of enhancment (arrows).

Figure 13. Dynamic-contrast enhancement patterns (Time/enhancement curves): the presence of a wash-out phase (i.e. a drop in signal intensity after a rapid initial contrast uptake – Type 2 or 3) is indicative of malignant disease.
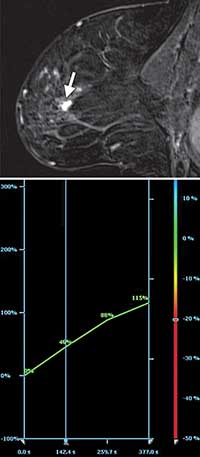
Figure 14. High-grade DCIS seen on a sagittal postcontrast subtraction image (top) shows an area of clumped NME measuring up to 2 cm (arrow) that demonstrated Type 2 enhancement kinetics (bottom).

Figure 15. High-grade DCIS appearing as a nodular-enhancing lesion on contrast-enhanced T1-w images. Enhancement kinetics (Type 1) was more in keeping with a benign lesion. An increase in size of the lesion was noted compared to a previous MRI scan, which prompted biopsy.

