Pitfalls in death certification
Kathleen England
|
Abstract Apart from their administrative purpose, death certificate data are a major means of identifying public health problems and evaluating the effectiveness of programs developed to deal with these public health problems. The inaccuracies in death certification are well documented in the international literature. This study aimed to estimate the accuracy in cancer death certification locally, as well as present common types of errors in order to create educational awareness. |
Introduction
Without health data, governments and other organisations cannot accurately target resources to prevent deaths and diseases, and have no way to measure whether their efforts are working.1 Mortality data obtained from information recorded on the death certificate is one of the oldest sources of health data. Published mortality data for Malta, by cause of death are available since 1872. These were produced in the form of a fortnightly report published by the Chief Police Physician. Annual reports after 1896 were published by the Chief Government Medical Officer.
Mortality data is a source of information used:
1. To monitor trends and patterns in disease;
2. To guide health promotion, resource allocation, service planning and priority determination;
3. For research and epidemiology; and
4. For administrative purposes including settlement of estates, welfare and pension entitlements and insurance payment.2
Mortality statistics are mainly based on the ‘underlying cause of death’ which is defined as “(a) the disease or injury which initiated the train of morbid events leading directly to death, or (b) the circumstances of the accident or violence which produced the fatal injury”.3 This is because from the standpoint of prevention of death, it is necessary to break the chain of events or to effect a cure at some point. The most effective public health objective is to prevent the precipitating cause from operating.
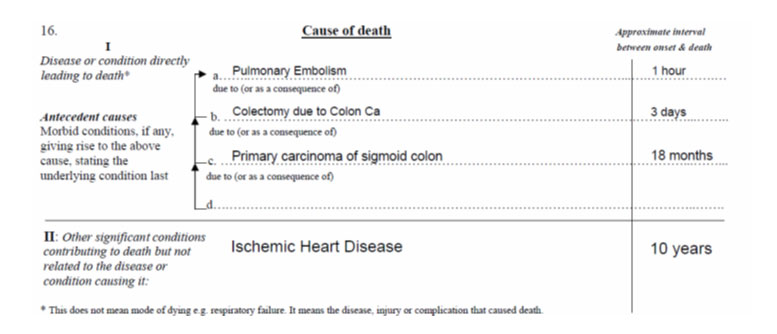
For this reason, section 16 of the Medical Death Certificate is divided into two parts with part I relating to the train of events leading directly to death, and part II concerns unrelated but contributory conditions. The condition recorded on the lowest used line of part I of the certificate is usually the underlying cause of death used for tabulation, if the death certificate is completed accurately.
Figure 1. Example of a completed medical section of the death certificate
Despite the importance of accurate death certification, errors are common. International studies report inaccuracies in death certificates to be 20-65%.4,5 In a previous local study (by the author, unpublished), it was found that 37% of death certificates reviewed were found to have a major error which means that coders had difficulty in choosing the correct underlying cause of death. The variable which was most significantly associated with a major error rate was age of the deceased.
Aim
The aim of the study was to review all death certificates in 2013 and estimate the accuracy in cancer death certification. The common types of errors are presented in order to create educational awareness.
Methodology
All death certificates of deaths registered during 2013 were reviewed and the main cause of death according to the certifier was extracted. Where the main cause of death was certified to be cancer, the death certificate was reviewed and additional information obtained by linking with the National Cancer Registry, seeking histology and radiological information from ISOFT and accessing the electronic case summary of the patient to confirm or otherwise the cancer and the underlying cause of death.
Results
In all there were 888 death certificates which were classified as a cancer death i.e. a particular cancer was recorded by the certifier as the main or underlying cause of death. Of these, 796 certificates or 89.6% were confirmed to be correct. As seen in table 1 below, the error rate increased with age of the deceased. This is attributed to the fact that often in the elderly, competing causes may exist and the certifier may be unsure what was the main or underlying cause of death.
Table 1. Number and % of major errors in cancer death certification
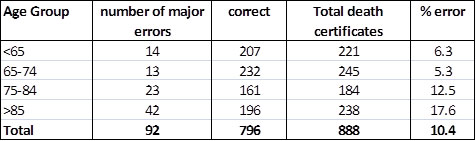
The percentage of incorrectly completed death certificates involving a cancer as a main cause was higher in death certificates certified by general practitioners compared to those certified by hospital doctors (14% versus 10%). This can be generally attributed to less accurate information being available to the general practitioner versus the hospital doctor. Furthermore, the proportion of death certificates certified by general practitioner increases in the elderly and decreases for hospital doctors.
The main errors identified were:
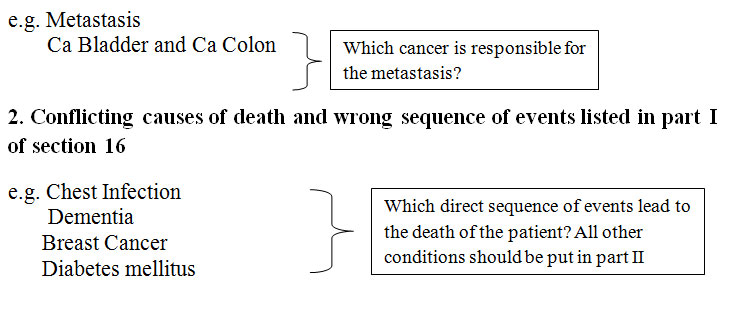
3. Wrong cancer written down on the death certificate
· “Metastasis” without identification of primary site should only be written when there is no known primary site and this should be stated.
· When there is metastasis to the lung, the certifier should write “Metastasis to the lung with unknown primary”. In this case, reporting “Carcinoma Lung” is incorrect as the coder would not know if it is a primary or due to metastasis.
· “Carcinoma oesophagus” should not be written when the primary site of the carcinoma is the stomach.
· When writing “liver cancer” one should always specify whether it is primary or secondary.
4. No evidence of cancer
In a few of the certificates reviewed, especially in elderly persons, there was
mention of a cancer with no evidence found by the coder.
A number of other minor errors have also been identified which include absence of time intervals between onset and death and lack of specificity about the tumour. E.g. “Adeno-carcinoma of the sigmoid colon” should be written rather than “cancer of the colon”; “Left frontal lobe primary malignant tumour of brain consistent with astrocytoma” should be written instead of “brain tumour”.
Discussion and conclusions
In a previous local study (by the author, unpublished), high levels of agreement between the certifier and the medical notes were found for neoplasms (92%), cerebrovascular disease (92%) and chronic lower respiratory diseases (86%). Lower levels of agreement were found for Ischaemic heart disease (78%), pneumonia (58%) and diabetes mellitus (31%).
The reported rate for neoplasms (92%) is similar to that found in this study (89.6%) and highlights the fact that deaths from neoplasms tend to be more straightforward than other conditions which involve multiple co-morbidity.
Often physicians enter correct diagnoses on the death certificate in an incorrect fashion. The reasons for this are many, but most commonly involve problems in distinguishing among the underlying cause of death, the immediate cause of death, the manner of death, and conditions contributing to death.6
Age is often associated with increase in major errors. Aging is often accompanied by the development of degenerative and chronic processes that affect many body systems. The question then arises as to which of the several co-existing conditions caused death. The clinician may logically say that none of the diseases singly, but rather a combination of conditions, caused the patient’s death.7 However it must be remembered that the attending physician is the one individual best able to prioritize the medical history in order to determine, in his or her best judgment, what disease process initiated the sequence of events leading to death.6
Doctors may find difficulty in completing a death certificate and distinguishing among the underlying cause of death, the immediate cause of death, the manner of death and conditions contributing to death. The increase in availability of electronic patient health data to doctors, especially general practitioners, is an important tool for reporting more specific information e.g. exact type of cancer.
While ad hoc training into the completion of the death certificate has been undertaken several times by the Directorate for Health Information and Research, death certificate completion is not included in any structured training programme for post-graduate doctors and new teaching tools need to be developed to reach as many doctors as possible in an on-going fashion.
References
1. Bloomberg M, Bishop J (2015). Understanding death, extending life. The Lancet, October 17, 2015 Vol: 386.
2. McAllum C, St. George I, White G (2005). Death certification and doctors’ dilemmas: a qualitative study of GPs’ perspectives. British Journal of General Practice 2005; 55:677-683.
3. World Health Organization. Instruction Manual of the International Statistical Classification of Diseases and Related Health Problems, tenth revision, Geneva 1992.
4. McKelvie P (1993). Medical certification of causes of death in an Australian metropolitan hospital. Comparison with autopsy findings and a critical review. Med J Aust 1993; 158: 816-821.
5. Slater DN. Certifying the cause of death: an audit of wording inaccuracies. J Clin Pathol 1993; 46:232-234.
6. Kircher T, Anderson RE (1987). Proper completion of the death certificate. Journal of the American Medical Association 1987; 258:349-52.
7. Erhardt C (1958). What is ‘the cause of death’? Journal of the American Medical Association 1958; 168:161-168.


