Colour of phlegm can predict outcomes for patients with the lung disease, bronchiectasis
Milan, Italy: The colour of the phlegm from patients with the lung disease bronchiectasis can indicate the degree of inflammation in their lungs and predict their future outcomes, according to new research presented at the European Respiratory Society International Congress in Milan, Italy.
The study of nearly 20,000 patients from 31 countries is the first time that the colour of phlegm (also known as sputum) has been shown to provide clinically relevant information that reflects prognoses and, therefore, can aid decisions about treatment.
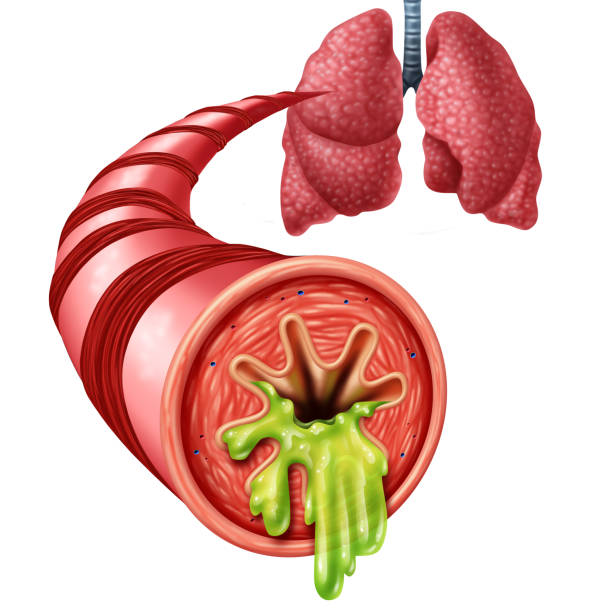
Bronchiectasis is a long-term condition for which there is no cure. One or more of the tiny branching airways, known as bronchi, widen and this leads to a build-up of excess mucus that can make lungs more vulnerable to infection. Over time, this can lead to gradually worsening damage to the lungs. Causes can include having a lung infection such as pneumonia or whooping cough, cystic fibrosis, underlying problems with the body’s immune system that make the bronchi more vulnerable to infection, or aspergillosis – an allergy to a certain type of fungi that causes the bronchi to become inflamed if fungi spores are inhaled. Bronchiectasis is one of the three most common chronic inflammatory airway diseases (along with asthma and COPD); it is prevalent in between 67 to 566 per 100,000 inhabitants in Europe, North America, the UK and the USA, and it can affect people of any age, although symptoms do not normally develop until middle age.[2]
Dr Megan Crichton, a postdoctoral researcher at the University of Dundee, UK, who presented the research, said: “One of the main characteristics of bronchiectasis is a productive cough, with almost three quarters of bronchiectasis patients producing sputum daily. When patients develop chest infections, their sputum colour darkens, and this colour change is due to a protein called myeloperoxidase or MPO, which is released from the inflamed cells; hence sputum colour can be used as a biomarker for inflammation.
“We know that the level of lung inflammation is important for long term health in bronchiectasis, so we wanted to know whether the sputum colour, when assessed when the patient is healthy with no chest infection, had any relationship to long-term outcomes such as lung function and frequency and severity of exacerbations.”
Dr Critchton and her colleagues recorded the sputum colour in 13,484 out of 19,324 patients who regularly coughed up sputum and who were enrolled in the pan-European bronchiectasis registry, EMBARC. They followed the patients for up to five years to look at the number of exacerbations they had, their severity and how many people died.
Sputum is classified into four levels: mucoid, which looks clear, frothy and grey-coloured; mucopurulent, which begins to show a creamy yellow colour; purulent, where the colour darkens into a dirtier yellow or green and the texture thickens; and severe purulent, which is the most severe and is a darker green turning into brown, sometimes including streaks of blood. Forty percent of the sputum-producing patients (5541) had mucoid sputum, 40% (5380) had mucopurulent, 18% (2486) had purulent, and 1% (177) had severe purulent sputum.
Dr Crichton said: “We found an increased risk of exacerbations, hospitalisations and death with more purulent sputum. For each 1-point increase in sputum purulence, there was a 12% increased risk of death.”
She continued: “As this is a large study conducted across multiple countries and with five years of follow-up data, it provides the evidence that sputum colour reflects prognosis. Sputum samples can be easily collected from most patients, and the colour has shown to be a useful indicator, thereby making sputum a readily available and easy-to-interpret clinical biomarker for disease progression. We believe that implementation of this biomarker into clinical practice will improve treatment and monitoring of bronchiectasis patients.
“Sputum sampling is non-invasive for patients, and they are actively encouraged to cough up sputum whenever possible to improve their lung function. Knowing that by looking at their sputum colour as a means of self-monitoring and self-management can empower patients and gives them some control over their condition, which we know is important for improving patient quality of life.”
The researchers are investigating introducing the sputum colour chart into clinical practice and the best way of helping patients to use it to monitor their own disease severity. They will be reporting these further findings in order make patients, clinicians and researchers aware of them.
Professor Carlos Robalo Cordeiro is President of the European Respiratory Society, Dean of the Faculty of Medicine at the University of Coimbra and Head of the Pneumology Department at Coimbra University Hospital, Portugal, and was not involved with the research. He said: “The findings from this study offer doctors and patients an easy, non-invasive way of monitoring their symptoms. If this is rolled out into clinical practice, it could make a real difference to managing this disease, and allow clinicians to intervene at an earlier stage if it becomes clear from the change in sputum colour that patients’ symptoms are worsening.”
Full bibliographic information
Published on 06/09/2023 by European Respiratory Society (ERS)
About: “Sputum colour assessment and clinical outcomes in bronchiectasis: data from the EMBARC Registry”
Authors: Dr Megan Crichton et al.
Additional Source
[1] Abstract no: PA397. “Sputum colour assessment and clinic Megan Crichton et al. Poster session, “Bronchiectasis registries, cohorts and subgroups” at 08.00-09.30 hrs CEST on Sunday 10 September 2023.
Link: https://k4.ersnet.org/prod/v2/Front/Program/?e=379&session=16436
[2] “The significant global economic burden of bronchiectasis: a pending matter”, Wei-jie Guan, Xiao-rong Han, David de la Rosa-Carrillo, Miguel Angel Martinez-Garcia. European Respiratory Journal 2019 53: 1802392; DOI: 10.1183/13993003.02392-2018
Journal link: https://erj.ersjournals.com/content/53/2/1802392
[3] See colour chart. Sputum colour: a useful clinical tool in non-cystic fibrosis bronchiectasis. Murray et al, Eur Respir J 2009, DOI: 10.1183/09031936.00163208
Journal Link: https://erj.ersjournals.com/content/34/2/361