Imaging Breast Implant Rupture
Dr Pierre Vassallo – Breast augmentation is the most common form of cosmetic surgery performed today. Most procedures involve the insertion of silicone gel-filled prostheses, which are selected for size and contour based on the woman’s body habitus and preference.
The first gel-filled breast implants were developed in the early 1960’s, however these suffered from high material failure rates and were initially thought to be linked to connective tissue disorders. Major redesigns and material improvements have lead to the development of 4th and 5th generation implants that have semi-solid silicone filler-gel and a strong silicone capsule. These new implants have the advantage of retaining their original shape and have a lower risk for rupture.
Implant rupture is the most common complication of silicone breast implantation and is more likely to occur with increasing implant age. This is due to weakening of the implant shell; the mean implant life span has been reported to be 13 years.1
Due to its semi-solid consistency, rupture of a silicone-filled implant may cause no symptoms and may be incidentally noticed during breast imaging studies. This contrasts with rupture of water-filled implants, which deflate rapidly producing a dramatic change in breast shape. Clinical findings of silicone breast implant rupture, when present, may include changes in breast size or shape, a palpable abnormality in the breast or axilla, pain, or skin tightening.2
Mammography does not cause implant rupture; anecdotal cases of this occurrence are likely due to implant leak that occurred prior to the mammographic examination.3
A fibrous capsule forms around the implant’s shell; this represents the body’s attempt to wall itself off from the foreign object; this fibrous capsule creates a barrier that has important implications in limiting flow of free silicone in case of implant rupture. A rupture that involves the implant shell with an intact fibrous capsule is called an intracapsular rupture (Fig 1b), while breakdown of the fibrous capsule with extravasation of silicone into the adjacent tissues is known as an extracapsular rupture (Fig 1c). Around 85% of implant ruptures are of the intracapsular type and most will cause no clinical symptoms or signs. Extension of silicone outside the capsule may induce an inflammatory response that may cause pain and local deformity.
Diagnosis of implant rupture with mammography, ultrasound and Magnetic Resonance Imaging (MRI) has been described in several articles; the advantages of each imaging modality will be discussed below.
Mammography
Mammography is the least sensitive breast imaging modality for implant rupture. This results from the high density of silicone that prevents internal analysis of the implant. However, evaluation of the contours of a breast implant may indicate a problem with implant integrity (Fig 2a); it is particularly useful to compare with previous exams when analysing changes in implant contour.
Intracapsular tears are mostly missed by mammography. A rounded implant shape may indicate capsular contracture but does not indicated rupture. Calcifications within the capsule occur with older long-standing implants and are not indicative of rupture.
Mammography is useful for detecting an extracapsular rupture since there is extravasation of silicone into the surrounding breast tissue (Fig 3). However, careful attention must be given in the case of a replaced implant, since free silicone will persist within the soft tissues from a previous implant leak. An extracapsular leak may result in silicone collecting within the axillary lymph nodes. However, small amounts of silicone in axillary lymph nodes may result from a process known as “gel-bleed” and are not a sign of implant rupture; gel-bleeds occur when freed silicone molecules that were not fully bound within the polymer capsule leak into surrounding tissues and are transported to regional lymph nodes.
The primary purpose of mammography is to screen for breast cancer; it should not be used to detect implant rupture.
Ultrasound
Breast ultrasound is superior to mammography for detection of breast implant leaks but less accurate than breast MRI. Given the wide availability and low cost of breast ultrasound compared to breast MRI, it has become a very important tool. Since its negative predictive value for detecting leaks is high,4 breast ultrasound is often used as a first examination before proceeding to MRI for more accurate assessment of prosthesis integrity.
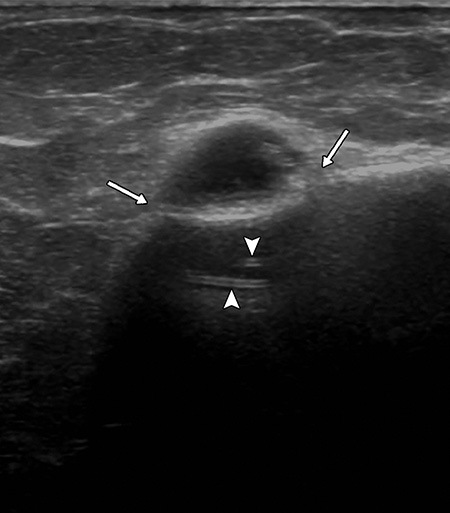
A single lumen silicone implant appears anechoic with no internal features on ultrasound. Implants fold themselves within the surgical pocket created by the plastic surgeon; these folds should not be mistaken for implant leaks. With time, a fibrous capsule forms around the implant; this capsule and the implant shell form a capsule-shell complex that appears as three parallel echogenic lines on ultrasound (Fig 4).
Intracapsular leaks may appear on ultrasound as echogenic material deep to the capsule or as an interruption of the capsule-shell complex (Fig 5a). They may also present as echogenic material between the layers of the capsule-shell complex (Fig 5b). An intracapsular tear may also result in complex folding of the implant shell known as the step-ladder sign (Fig 5c). It is important not to confuse normal implant folds with an intracapsular leak.
An extracapsular leak presents as echogenic material (silicone) within the soft tissues of the breast with no delimiting trilaminar complex (Fig 6a). Free silicone may also be present in the axillary lymph nodes (Fig 6b).
Breast MRI
MRI is the most accurate imaging modality to assess breast implant integrity. In the US, the food and drug administration recommends a breast MRI 3 years after implant surgery and bi-yearly thereafter to monitor implant integrity. However, this is not universally accepted since there is no clear evidence that it will influence patient morbidity.
Careful questioning of patients prior to breast MRI is required; saline-filled implants do not require MRI evaluation, while the presence of tissue expanders (implants that can be filled by external injection of saline) are a contraindication to MRI, because they contain magnets at the injection port. Only silicone-filled implants should undergo MRI examination.
The augmented breast contains fat, water and silicone, and MRI can analyse each of these components separately clearly mapping each one within the breast. MRI sequences that null out fat and water clearly depict extracapsular silicone (Fig 7a), while sequences that null out silicone can distinguish a silicone leak from a fluid collection (Fig 7b).
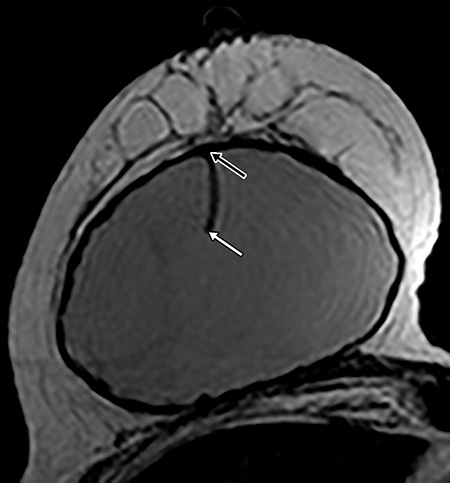
MRI allows accurate assessment of the posterior margin of the implant, which is difficult to see on ultrasound. Implant herniations through the capsule are best seen on MRI and although they do not constitute a leak, they will result in contour deformity (Fig 8a). The presence of free silicone between the implant shell and the capsule can readily confirm an intracapsular rupture (Fig 8b). On the other hand, the classical “linguine” sign, which correlates with the complex folds of the collapsed implant shell, may also occur with intracapsular rupture (Fig 8c).
Extracapsular tears and the presence of free silicone in the axillary tissues and lymph nodes can be readily evaluated with silicone selective MR imaging (Fig 9). Implant assessment MR protocols must be clearly distinguished from breast cancer screening protocols. The latter require injection of intravenous contrast agent. However, both protocols can be combined if required, delivering the best analysis of implant integrity and the most accurate screening method for breast cancer.
Extracapsular silicone leaks may sometimes mimic breast cancer on mammography and ultrasound; breast MRI can distinguish the two entities and therefore is a valuable tool when assessing patients with a high-risk for breast cancer who have had breast augmentation.
The new generation of breast implants are composed of semi-solid silicone gel (cohesive or “gummy bear” implants). These designs are aimed at reducing the risk of free silicone migration into soft tissue. These implants have been noted to fracture rather than leak; these fractures are best evaluated with breast MRI.
Conclusion
Breast imaging is one of the most commonly performed diagnostic imaging studies. Although breast imaging is mainly aimed at detecting early breast cancer, an increasing number of women who attend breast cancer screening have had breast augmentation procedures. It is important to recognise the radiological findings related to breast implant leaks as they may mimic breast cancer. Breast implant imaging is also important when planning management of implant leaks.
Figure Legends
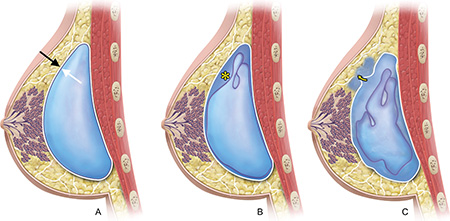
Figure 1: a. Intact implant showing capsule (black arrow) and implant shell (white arrow). b. intracapsular rupture with silicone (*) present between the capsule and the shell. c. extracapsular rupture with silicone extravasating (arrow) outside the capsule.
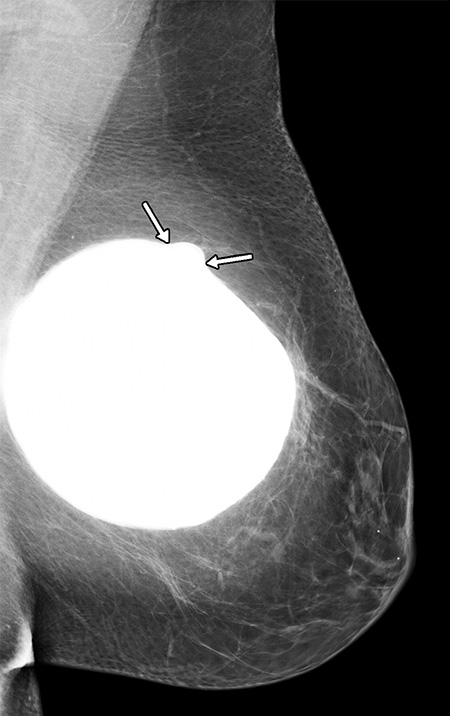
Figure 2: a. Mammogram showing an abnormal implant contour (arrows).
b. Ultrasound confirms an intracapsular rupture with silicone leak (arrows) and a displaced shell depicted as parallel echogenic lines (arrowheads).
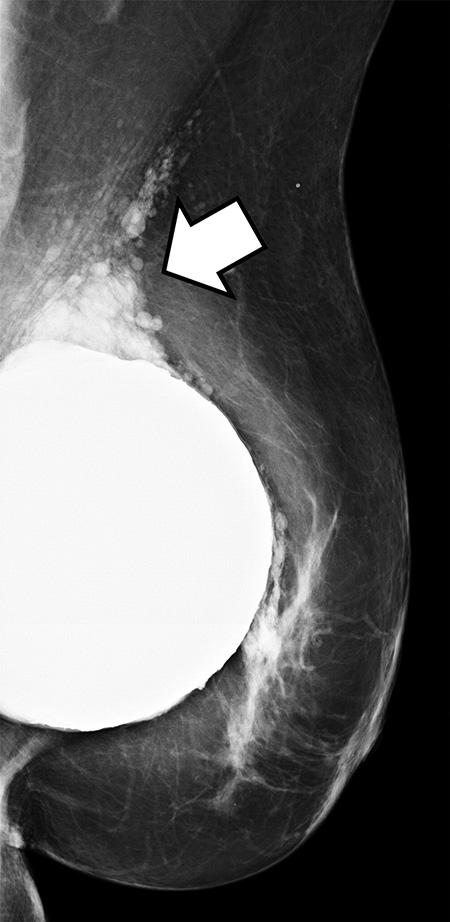
Figure 3: Extravasation of silicone into breast tissue (arrow) confirming an extracapsular implant leak.
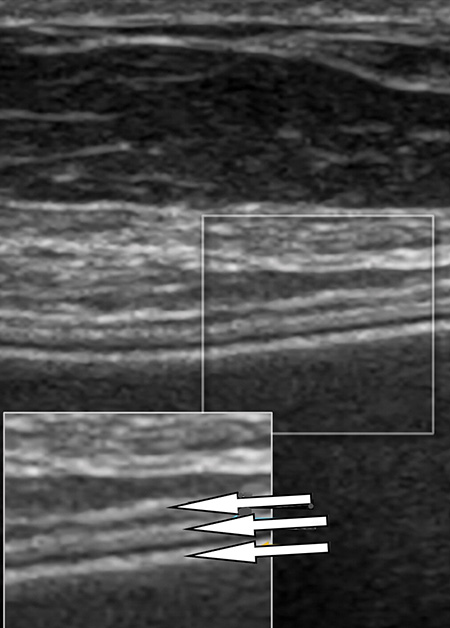
Figure 4: The trilaminar structure (arrows) of the shell-capsule complex seen on ultrasound.
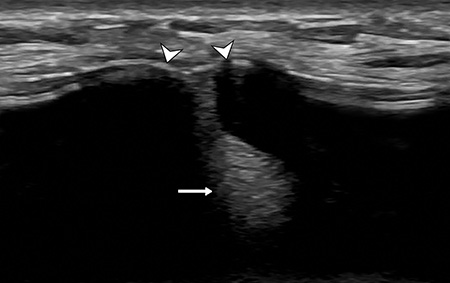
Figure 5: a. Ultrasound shows echogenic material (arrow) deep to the capsule-shell complex and loss of the trilaminar structure of the capsule-shell complex (arrowheads).
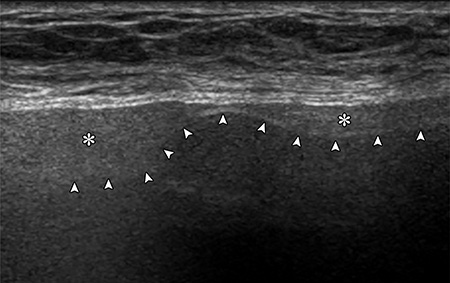
b. Ultrasound showing echogenic material (*) between the layers of the capsule-shell complex (displaced shell shown with arrowheads).
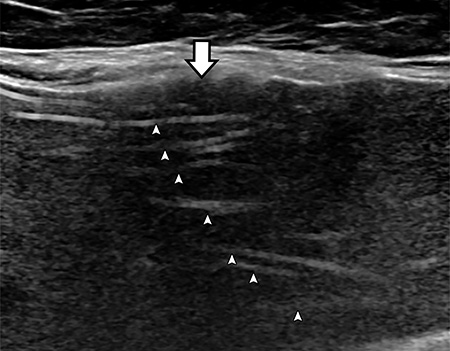
c. Ultrasound showing complex folding of the implant shell (arrowheads) known as the step-ladder sign and disruption of the trilaminar capsule-shell complex (arrow).

Figure 6: a. Ultrasound showing echogenic material (*) within the soft tissues of the breast with no limiting capsule-shell complex (arrows), which confirms an extracapsular leak.

b. Ultrasound showing an axillary lymph node (between arrows) containing echogenic free silicone (*).
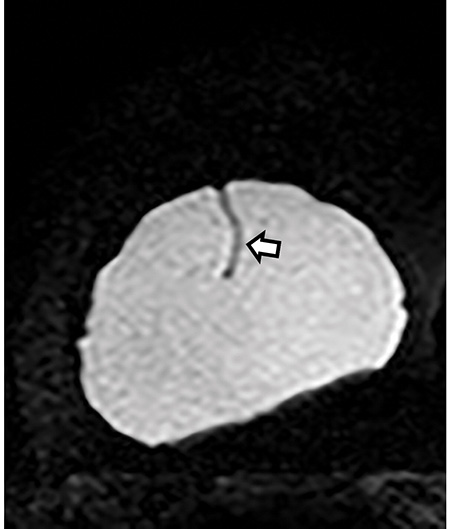
Figure 7: a. A silicone only MR image showing a normal fold in the implant shell (arrow).
b. A T2-weighted MR image showing low fat signal and intermediate silicone signal depicting a detailed breast tissue anatomy.
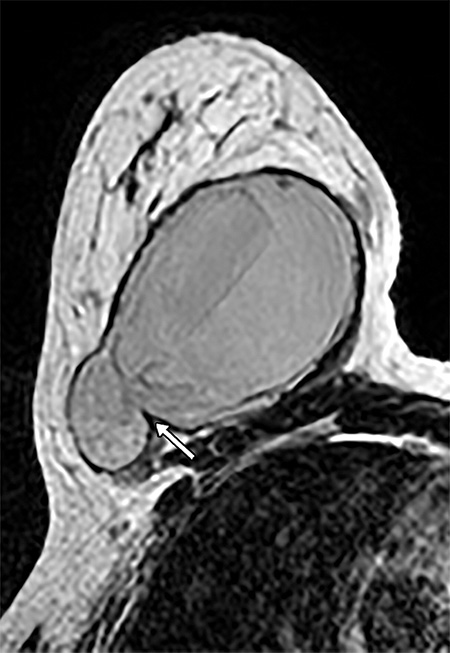
Figure 8. a. Implant herniation (arrow) seen on this T2-weighted MR image.

b. T2-weighted MR showing free silicone (*) between the capsule and the implant shell (arrows).
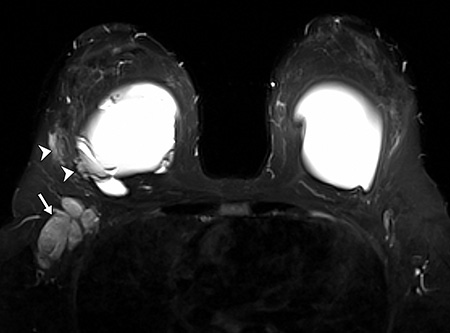
Figure 9: MR silicone image showing an extracapsular rupture (arrowheads) in the lateral aspect of the right breast and silicone within the right axillary lymph nodes (arrow).
References
- Rohrich RJ, Adams WP Jr, Beran SJ, et al. An analysis of silicone gel-filled breast implants: diagnosis and failure rates. Plast Reconstr Surg 1998;102(7):2304–2308; discussion 2309.
- Hölmich LR, Fryzek JP, Kjøller K, et al. The diagnosis of silicone breast-implant rupture: clinical findings compared with findings at magnetic resonance imaging. Ann Plast Surg 2005;54(6):583–589.
- Juanpere S, Perez E, Huc O, et al. Imaging of breast implants: a pictorial review. Insights Imaging 2011;2(6):653–670.
- Venta LA, Salomon CG, Flisak ME, et al. Sonographic signs of breast implant rupture. AJR Am J Roentgenol 1996;166(6):1413–1419.

