Imaging Groin Hernias
by Pierre Vassallo
Clinical differentiation of direct inguinal hernias, indirect inguinal hernias, femoral and Spigelian hernias can be difficult particularly with small hernias and in obese patients. Diagnostic imaging can detect and characterize hernias more reliably, allow better surgical planning and possibly even prevent unnecessary surgery. Detection of complications occurring in groin hernias is also of importance. Hernial incarceration is particularly evident on ultrasound (US) performed during rest and abdomimal straining (Valsalva maneuver) in both the supine and erect postures. Hernial strangulation is visible both with US and with computed tomography (CT) with fluid appearing around the hernial sac contents.
Detecting and characterizing groin hernias with cross sectional imaging techniques requires an accurate knowledge of regional anatomy and particularly of the landmarks that can help identify the type of hernia.
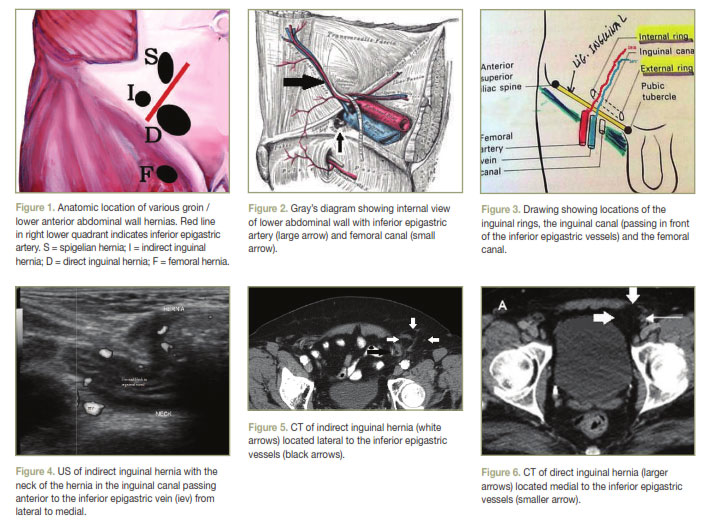
Figure 1 shows a schematic image of the anterior abdominal wall with the locations of four types of groin hernias that are commonly encountered in clinical practice: direct and indirect inguinal hernias, femoral hernias and spigelian hernias. The two important landmarks indicated here are the inferior epigastric artery and the inguinal ligament.
The inferior epigastric artery originates from the external iliac artery within the pelvis and extends superiorly and medially towards the umbilicus coursing deep to the peritoneum that lines the internal aspect of the lower abdominal wall (Figure 2). The second important landmark is the inguinal ligament. The groin can thus be divided into the supra and infra-inguinal compartments and the supra-inguinal compartment is further divided into medial and lateral compartments.
Indirect inguinal hernias pass through the inguinal canal along with the spermatic cord in males or the round ligament in females. They enter through the internal inguinal ring into the inguinal canal and exit through the external inguinal ring (Figure 3). The internal inguinal ring lies lateral to the inferior epigastric artery, so an indirect inguinal hernia enters the abdominal wall lateral to the said artery and courses medially anterior to it. US and CT can visualize the inferior epigastric artery and also the neck of the hernial sac (Figures 4 & 5) lying lateral and then anterior to the said artery. Indirect inguinal hernias are five times more common than direct hernias. In boys, indirect inguinal hernias are the result of a congenital defect of a patent processus vaginalis. In adults, they are acquired due to weakness and dilatation of the internal inguinal ring.
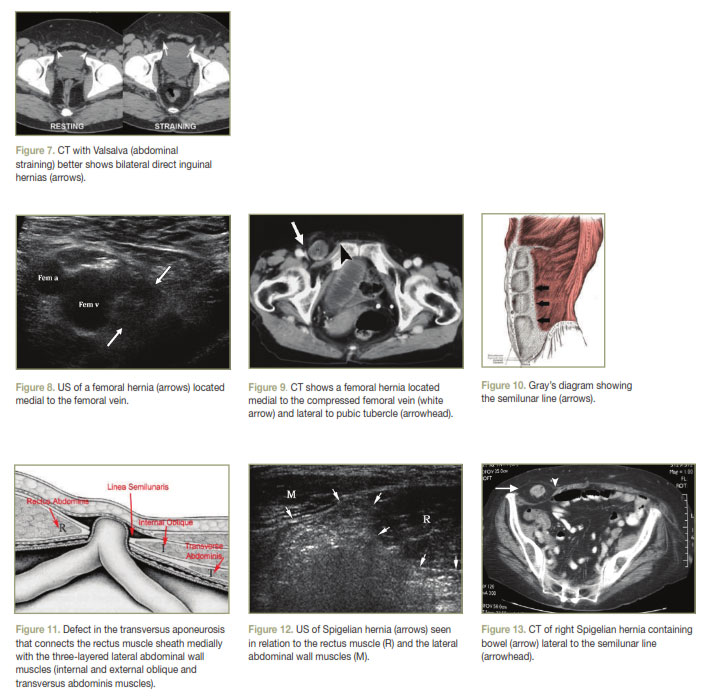
A direct inguinal hernia emerges medial to the inferior epigastric artery passing directly through the posterior wall of the inguinal canal into the external inguinal ring. Weakness of the posterior wall in the inguinal canal may be congenital or acquired, in the latter case due to excessive abdominal wall strain. Both US and CT can identify the inferior epigastric artery (Figure 6) as well as the orientation of the neck of the hernia sac relative to the inguinal ligament. Valsalva maneuver performed during US or CT will help identify spontaneously reducing inguinal hernias that are commonly bilateral (Figure 7).
Femoral hernias exit below the inguinal ligament and protrude through the femoral ring medial to the femoral vein and artery in the femoral canal; they lie medial to the common femoral vein which they often compress (Figures 8 & 9). Femoral hernias are relatively uncommon, with a prevalence less than one-tenth that of inguinal hernias. They have a female predominance of 4:1, which is thought to be secondary to dilatation of the femoral ring connective tissues due to the hormonal and physical changes of pregnancy. For unclear reasons, femoral hernias are twice more common on the right than on the left.
Spigelian hernias are distinct from inguinal and femoral hernias in that they are not related to the inguinal canal or the inguinal ligament. However their relative proximity to the aforementioned hernias and their relative frequency particularly in the young sportive population makes them worth mentioning here. Spigelian hernias occur through a slit-like defect in the anterior abdominal wall adjacent to the semilunar line (Figure 10) that runs along the lateral margin of the rectus abdominis muscle. Most spigelian hernias occur in the lower abdomen where the posterior sheath of the rectus abdominis is deficient. The hernia ring is a well-defined defect in the transversus aponeurosis (Figure 11). Both US (Figure 12) and CT (Figure 13) are capable of visualizing spigelian hernias, establishing their contents and detecting complications.
Hernias could contain virtually any organ or tissue found in the lower abdomen. These may include but are not limited to fat, small or large bowel, a portion of the bowel wall (Richter hernia), omentum, incarcerated appendix (Amyand hernia), bladder, Meckel diverticulum (Littré hernia), and gonads. Femoral hernias are the most likely to strangulate, whereas direct inguinal hernias are the least likely to complicate. Other complications include intestinal obstruction, incarceration, volvulus, perforation, appendicitis or diverticulitis, and tumors that may be found incidentally in the hernia.
CT and US are useful for detecting all the above hernias and their complications to allow timely surgical planning.