Large intestinal (Colorectal) Cancer Screening
Pierre Vassallo
T he large intestine is composed of the colon and rectum and is the third most common site of cancer in the body. Colorectal cancer affects both males and females equally and is the second most common cause of death from cancer.
Screening for colorectal cancer can reduce deaths from this condition significantly.1 The aim of screening is to detect precancerous/cancer-prone lesions before they become malignant. Screening methods include Faecal Occult Blood Testing (FOBT), Double Contrast Barium Enema (DCBE), Computed Tomographic Colonography (CTC) and Colonoscopy.
FOBT looks for blood in the stool, but it has been shown to be unreliable as it misses non-bleeding cancers (false negatives) and is unable to distinguish cancer from other (non-cancerous) causes of intestinal bleeding (false positive).2
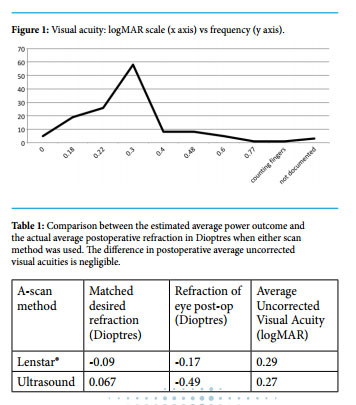
DCBE is an X-ray examination that involves coating the large bowel with barium sulphate-based contrast material and distending it with air followed by a series of X-ray images to view different portions of the colon and rectum (figure 1). DCBE has been used for many years and is a reliable tool for detecting colorectal cancer, however it has largely been replaced by CTC. CTC offers numerous advantages, namely, 3D viewing of the colon, detection of disease within the colonic lumen, as well as in the colonic wall and beyond , while also viewing potential sites of cancer spread (metastasis) particularly the liver and lymph nodes. DCBE is also of limited value in those patients in whom bowel preparation measures fail to attain adequate bowel cleansing.
FOBT looks for blood in the stool, but it has been shown to be unreliable…
CTC uses the advantages of Computed Tomography to deliver high resolution 3D and cross-sectional images of the large bowel, while allowing analysis of all other abdominal and pelvic organs. Prior to the examination, bowel cleansing measures are taken in order to improve visibility of abnormalities in the bowel wall. Bowel preparation usually lasts 2 days, in which laxatives and adequate hydration are prescribed using a standard protocol. Just prior to the CT examination, a short rectal tube is inserted and the colon is insufflated with air or carbon dioxide (CO2 ); CO2 is preferred as it is more rapidly absorbed and results in less discomfort due to bowel distention. Adequate bowel distention is confirmed through a prior scout image of the abdomen. Subsequently prone and supine CT scans using a multi-detector CT scanner (usually 64-slice scanners are used) are performed using a thin section technique with slices measuring 0.6mm or less in thickness. The supine scan is performed with intravenous contrast material injection. Electronic cleansing techniques have been developed that increase patient comfort and compliance by replacing pre-examination bowel preparation regimens; this is achieved by administering oral contrast material prior to the exam to label the faecal contents of the bowel, which can be subsequently electronically subtracted from the CT images.
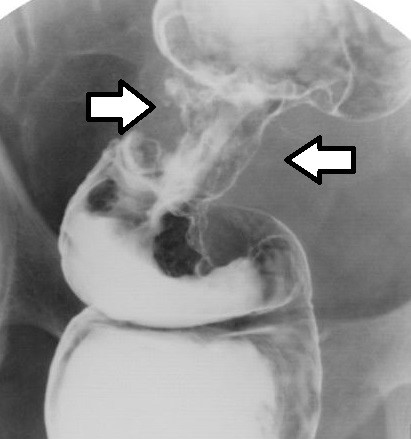
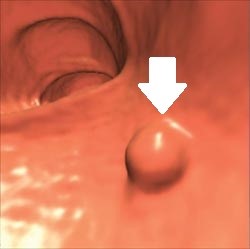
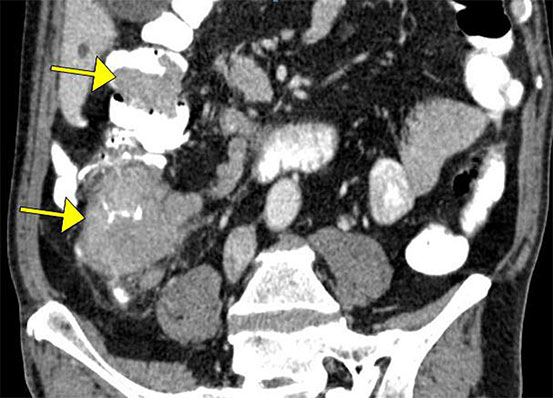
CTC exams are reviewed in 3D endoscopic mode (https:// youtu.be/8MiufJNDrU8) and in multi-planar cross-sectional mode. The 3D endoscopic mode allows visualisation of that portion of any abnormality that protrudes into the bowel, while the cross-sectional mode detects extension of disease through and beyond the bowel wall. CTC can visualise polyps and measure polyp size (figure 2). The extent of bowel wall penetration and local (figure 3) as well as distant metastatic disease (figure 4) can also be assessed.


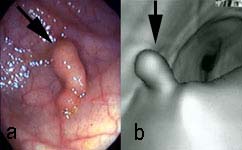
Colonoscopy is a procedure that allows visualisation of the inner lining of your large intestine. This is done by inserting a flexible colonoscope through the anus to look at the colon (figure 5). The procedure is performed in an operating theatre and usually requires light general anaesthesia. Sometimes colonoscopy is performed under sedation, however this is frequently not well tolerated by the patient. Prior meticulous bowel cleansing is required. Long and tortuous large intestines, which are often present in the elderly population, may prevent the examiner from viewing the more proximal portions of the colon; in this case, one would need to resort to performing a CTC. A colonoscopy allows direct visualisation of ulcers, colon polyps, tumours, and areas of inflammation or bleeding. During a colonoscopy, biopsies can be collected and abnormal growths can be taken out.
CTC has rates of polyp detection comparable to those of colonoscopy, and its use in favour of colonoscopy improves overall compliance of patients who should have regular colorectal cancer screening. It is minimally invasive, requires no sedation/anaesthesia, has the potential for reducing the number of incomplete examinations (inability to reach the proximal colon), and has faster patient throughput.2,3
The aim of any colorectal cancer screening test is to detect an advanced adenoma, which is pathologically defined as a lesion that is 10 mm or larger, has villous features, or has high-grade cellular dysplasia. Lesions smaller than 6 mm are often hyperplastic with no malignant potential. Adenomatous polyps that are 5 mm or smaller have a slow growth rate and a low incidence of dysplasia, and both CTC and colonoscopy have low sensitivity for depicting them. A reporting protocol for CTC known as the CT colonography-Reporting and Data System (C-RADS) recommends that these lesions should not be reported in view of the fact that the risk for malignancy in adenomatous polyps that are 5 mm or smaller is estimated to be much less than 1%.4 C-RADS recommends short-term surveillance for patients with one or two 6–9-mm polyps and no additional risk factors, although there is continued debate and research relating to the appropriate polyp size and number to determine whether to either opt for colonoscopy and biopsy or for a surveillance strategy.
The aim of colorectal cancer screening is to detect precancerous polyps and to remove them before they turn into cancer. Screening also helps to find colon cancer at an early stage, when treatment often leads to a cure. The incidence of colorectal cancer rises after 50 years of age. So after turning 50 or if experiencing abnormal bowel symptoms (such as an altered bowel habit or blood in the stools), one should get screened without delay. Colon cancer screening saves lives.