Major study shows prostate MRI reveals more cancers which need treatment, and reduces overdiagnosis compared to standard biopsy
A large international study has shown that an MRI scan can reduce the number of invasive prostate biopsies by up to 28%. The PRECISION1 trial shows that using MRI to target prostate biopsies leads to more of the harmful prostate cancers, and fewer harmless cancers being diagnosed. Given that more than a million men in Europe undergo a prostate biopsy every year, the authors believe that this work could change clinical practice. The results are presented today at the European Association of Urology Congress in Copenhagen, with simultaneous publication in the New England Journal of Medicine.
 Why is this important?
Why is this important?
Dr Veeru Kasivisvanathan of University College London and first author of the study, said:
“PRECISION is the first international multi-centre randomised trial to show the benefits of using MRI at the start of the prostate cancer diagnosis process.
In men who need to have investigation for prostate cancer for the first time, PRECISION shows that using an MRI to identify suspected cancer in the prostate and performing a prostate biopsy targeted to the MRI information, leads to more cancers being diagnosed than the standard way that we have been performing prostate biopsy for the last 25 years”.
Dr Caroline Moore, Reader in Urology at University College London and senior author of the study commented:
‘We compared standard prostate biopsy to the use of MRI, offering targeted biopsies to only those men who had a suspicious MRI. The MRI pathway detected more harmful cancers that needed treatment, and it reduced overdiagnosis of harmless cancers, even though fewer men had a biopsy in the MRI arm. ’
Professor Mark Emberton of University College London commented:
‘This study was the first to allow men to avoid a biopsy. If high quality MRI can be achieved across Europe, then over a quarter of the 1 million men who currently undergo a biopsy could safely avoid it’.
Background
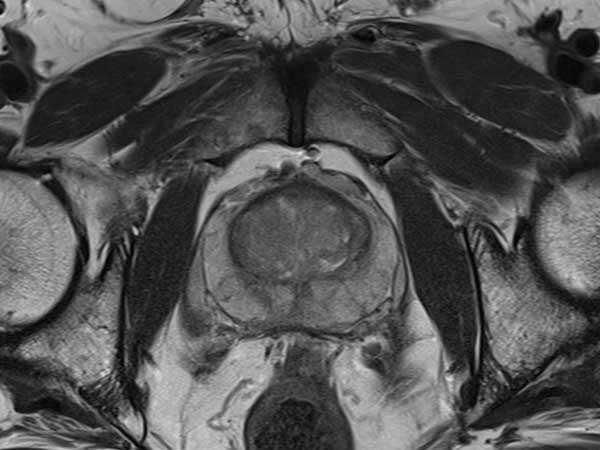
Prostate cancer is currently diagnosed by examining biopsy samples taken from the prostate via a procedure called TRUS (TRansrectal UltraSound guided prostate biopsy). This means taking around 10-12 samples from the prostate using a probe with a special needle. The ultrasound-guided procedure means inserting a probe into the anus under local anaesthetic. It is uncomfortable, costly, and carries a slight risk of infection, but because it involves estimating the position of a possible tumour, it also means that tumours are often missed. The PRECISION study investigates whether an MRI scan can avoid the need for biopsy in some patients, or give better diagnostic information where a biopsy is necessary.
What did they do?
Researchers from 23 centres randomly allocated 500 men to be examined either with a standard 10-12 core TRUS biopsy, or with an initial MRI scan followed by a targeted biopsy if the MRI showed an abnormality. The main aim was to assess what proportion of men were diagnosed with clinically significant prostate cancer (defined as a Gleason Grade of =3+4) which is harmful cancer that is desirable to find. It also aimed to assess the proportion of men who were diagnosed with clinically insignificant cancer (Gleason Grade 3+3) which is desirable to avoid as it doesn’t benefit from treatment.
What were the results?
The researchers found that 71 (28%) of the 252 men in the MRI arm of the study avoided the need for a subsequent biopsy. Of those who needed a biopsy, the researchers detected clinically significant cancer in 95 (38%) of the 252 men, compared with 64 (26%) of the 248 men who received only the TRUS biopsy.
“This shows that a diagnostic pathway with initial MRI assessment followed by biopsy when required, can not only reduce the overall number of biopsies performed, but can give more accurate results than TRUS-biopsy alone. We also found that patients who had MRI had fewer side effects than those who just had the standard TRUS biopsy. This is because the MRI allows some men to avoid biopsy and in those who need one, is able to better indicate which area of the prostate needs to be investigated, so you don’t need to randomly sample the whole prostate and can use fewer biopsy cores”, said Dr Kasivisvanathan.
What does this mean practically?
Several elements need to be considered for MRI to be generally adopted in the diagnostic process. As Dr Kasivisvanathan, who was awarded a National Institute for Health Research (NIHR), Research Doctoral Fellowship to carry out the study, said:
“The ability to perform good quality MRI and the ability to interpret the MRI information are specialist skills. We will therefore need appropriate training for clinicians to use the technology and changes in health services to increase availability and capacity to perform prostate MRI. In the long-term, this new diagnostic pathway can be cost-effective. Costs can be saved by the reduction in the number of men undergoing biopsy in the first place, by the earlier diagnosis of harmful cancers and in the avoidance of the diagnosis of harmless cancers”
Prostate cancer statistics
Prostate cancer is the most common male cancer, with around 400,000 new cases every year in Europe. In the UK, there are over 46,000 new cases of prostate cancer every year, leading to more than 11,000 deaths. 2015 figures show that for the first time there were more prostate cancer deaths than breast cancer deaths in the UK.
Commenting, Professor Hein Van Poppel, (EAU Adjunct Secretary General, University Hospitals of the Leuven), said:
“This is a significant study. Prostate cancer can only really be confirmed by a biopsy, which is invasive and, like almost all medical procedures, caries some risk of side-effects. Of course, in the majority of men who have a biopsy no cancer is found. This work shows that using MRI to decide whether or not to perform a biopsy has the potential to save around a quarter of a million European men each year from going through the biopsy procedure, and so may be cost-effective in the long run. MRI use also shows up small aggressive cancers at a curable stage, and allows us to delay or simply not perform biopsies for some cancers which will not turn out to be dangerous. We need time to digest the study, but at first reading it looks like it has the potential to change clinical practice”.
Source: European Association of Urology
Full bibliographic information:
The 33rd European Association of Urology conference




