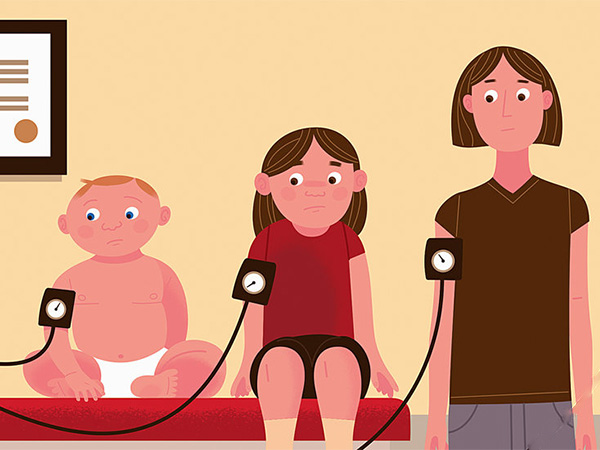
Many more people could benefit from blood pressure-lowering medication – most comprehensive study to date
Most detailed study to date including 345,000 people from 48 randomised clinical trials finds that blood pressure-lowering medication is effective in adults regardless of starting blood pressure level.
Each 5mmHg reduction in systolic blood pressure lowered the relative risk of cardiovascular events by around 10%, even in people with normal blood pressure and those who had never had a heart attack or stroke.
Authors call for global guidelines to be changed so that anyone with increased risk of cardiovascular disease is considered for blood pressure-lowering medication, irrespective of their blood pressure.
Blood pressure-lowering medication can prevent serious cardiovascular conditions such as strokes, heart failure and heart attacks even in adults with normal blood pressure, according to new research published in The Lancet.
Importantly, the study found the beneficial effects of treatment were similar regardless of the starting blood pressure level, in both people who had previously had a heart attack or stroke and in those who had never had heart disease.
The authors say that the findings have immediate and important implications for global clinical guidelines that typically limit blood pressure-lowering treatment to individuals with high blood pressure (usually above 140/90 mmHg).
“Our findings are of great importance to the debate concerning blood pressure treatment”, says lead author Professor Kazem Rahimi, University of Oxford, UK. “This new and best available evidence tells us that decisions to prescribe blood pressure medication should not be based simply on a prior diagnosis of cardiovascular disease or an individual’s blood pressure level. Instead, medication should be viewed as an effective tool for preventing cardiovascular disease in people at increased risk of developing heart disease or stroke. Clinical guidelines should be changed to reflect these findings.”
He cautions, “We’re not saying that everyone must begin treatment. The decision will depend on an individual’s risk factors for developing cardiovascular disease, the potential for side effects and patient choice.”
Heart disease and stroke, linked to high blood pressure, are the leading cause of death across most of the western world. It is widely accepted that blood pressure medication protects people who have had a prior heart attack or stroke from having a second, but the use of these drugs in people with normal or mildly elevated blood pressure has been debated . So far, studies examining whether blood pressure-lowering medication is equally beneficial in people with and without a history of cardiovascular disease, and at lower blood pressure levels than currently considered for treatment (typically 140/90 mmHg or higher) have reported conflicting findings. This has led to contradictory treatment recommendations around the world.
For the current analysis, the Blood Pressure Lowering Treatment Triallists’ Collaborators pooled data from 344,716 adults (average age 65 years) in 48 randomised trials (the gold standard for evaluating the effectiveness of treatments) to explore the effects of blood pressure-lowering medications. Participants were separated into two groups: those with a prior diagnosis of cardiovascular disease (157,728 participants – secondary prevention group) and those without (186,988 – primary prevention group, without cardiovascular disease).
Each group was then divided into seven subgroups based on levels of systolic blood pressure at study entry (less than 120, 120-129, 130-139, 140-149, 150-159, 160-169, 170 and above mmHg). Around 20% (31,239) of participants with prior cardiovascular disease and 8% (14,928) of those who had never had cardiovascular disease had normal or high-normal systolic blood pressure at the start of the trials (systolic blood pressure less than 130 mmHg).
Over an average of four years follow-up, 42,324 participants had at least one major cardiovascular event (heart attack, stroke, heart failure, or death from cardiovascular disease). For every 5 mmHg reduction in systolic blood pressure, the risk of developing major cardiovascular disease fell by around 10% (18,287 vs 24,037 major cardiovascular disease in the intervention and comparator groups, respectively), stroke by 13% (6,005 vs 7,767), heart failure by 13% (3,249 vs 4,584), ischaemic heart disease by 8% (8,307 vs 11,145), and death from cardiovascular disease by 5% (4,825 vs 6,110).
The beneficial effects of the treatment did not differ based on a history of having had cardiovascular disease or the level of blood pressure at study entry.
“It is important that people are considered for blood pressure-lowering treatment based on their cardiovascular risk, rather than focusing on blood pressure itself as a qualifying factor for or target of treatment,” says co-author Zeinab Bidel from the University of Oxford, UK. “We must provide well-rounded guidelines to lower risks for cardiovascular disease that include exercise, nutrition, smoking cessation, and – where appropriate – medication.”
The study has some limitations including that it only investigated the impact of starting blood pressure and prior cardiovascular disease on treatment effects, so the findings cannot be generalised to other patient characteristics that we have not included in our analysis. Additionally, the effects on diseases other than major cardiovascular disease, including potential side effects of treatment, were not specifically examined.
Source: The Lancet
Full bibliographic information