Meningococcal B vaccination: a novel approach

Published Ahead of Print
Prof. Simon Attard Montalto
 Abstract
Abstract
Meningococcal B disease is associated with a mortality of up to 10% and significant morbidity in survivors. Attempts to produce an effective vaccine based on established methods over several decades, have succeeded in designing vaccines suitable only for local and strain-specific outbreaks. To date, the 4CMenB vaccine is the first preventative measure that is effective on a global endemic level and could potentially cover against 80% of isolates that cause this devastating disease. Although costly, this vaccine appears to be safe and can be given with other vaccines. Early trials of a 3+1 infant schedule have shown encouraging levels of seroprotection at 13 months of almost 100% for all four vaccine components. Results from widespread national programmes have shown uptake levels for the vaccine in excess of 95% of the target population, and significant reductions in invasive meningococcal B disease by more than 50% of cases within just 10 months of starting the programme. Long term surveillance for late adverse events and to determine the duration of protection is ongoing, and countries will need to independently establish the cost-benefit and feasibility of a 4CMenB programme.
Introduction
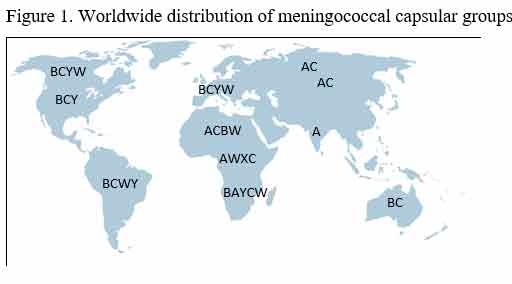
Although relatively uncommon, invasive meningococcal disease (IMD) is one of the most deadly infections affecting healthy infants, children and young adults. Out of a total of 12 circulating capsular groups of Neisseria meningitidis, just 6 account for over 90% of significant infection1. In Europe, North America and Australasia, most of these cases are due to meningococcal capsular group B and, to a lesser extent, group C organisms, whereas group A is endemic in Africa (Figure 1)2. Silent nasopharyngeal carriage of N. meningitidis can be as high as 10% within the adult population during the ‘cold and flu season’, increasing the risk of transmission especially from persons in close contact in confined spaces. Although this accounts for the ‘case clusters’ during social events, amongst army recruits and university students3, most cases are sporadic and the reason why some individuals appear to be more susceptible and go on to develop invasive disease is not clearly understood. Invasion occurs after a short incubation period of an average of 4 days (range 2-10 days) and, in the majority of cases, results in meningitis, septicaemia or both. The inherent severity of these conditions, combined with a fulminating course associated with an immunological cascade with serious complications including disseminated intravascular coagulation, shock and cardiovascular collapse, results in an overall case fatality rate of around 5-15%4,5. In those who survive, significant long term morbidity is present in around 10-20% and includes loss of digits and/or limbs, renal failure, blindness, deafness, cerebral palsy, cognitive impairment and epilepsy5.
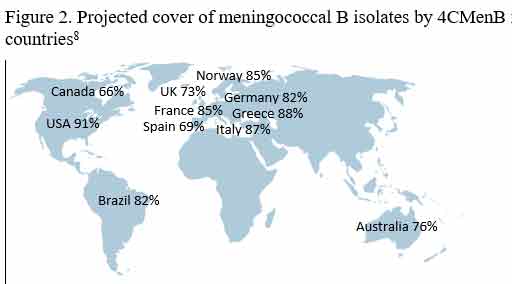
The rapidity of the infection and alarmingly high mortality and morbidity have ensured that meningococcal disease retains a high profile within medical circles as well as the general public. A significant amount of effort and resources have been directed to treat the acute illness, but also to prevent disease in the first place through vaccination. This has been very successful for some capsular groups including Men A6 and C7, but has been singularly difficult with regard to Men B disease where organism-derived antibody-inducing antigens within existing vaccines closely resemble human antigens and are, therefore, recognised as ‘self’ and render these vaccines non-immunogenic8. After decades of disappointment with early vaccines, a totally novel approach was required and this has now been successful in creating a vaccine that generates protection against 66-92% of circulating capsular group B N. meningitidis strains9.
Discussion
The burden of disease
In 2012, surveillance by the European Centre for Disease Prevention and Control (ECDC) confirmed that IMD comprised 43% meningitis, 29% septicaemia, 21% combined meningitis and septicaemia and the remaining 7% included septic arthritis, pneumonia, conjunctivitis, cervicitis, pericarditis and endocarditis10. This pattern of disease is true for both meningococcal B and C, although septicaemia is more common with group Y (50% versus 30% meningitis alone and 10% combined), whilst both meningitis and septicaemia comprise 40% of cases for group W and 45% for group A (versus 25% with meningitis and 15% septicaemia alone)11.
IMD generally affects infants and, to a lesser extent, preschool-age children, adolescents and young adults. This is true both for epidemics and during natural background infection. For example, during the Men B epidemic in New Zealand over 1991-96, the incidence was 142/100,000 in infants and 73/100,000 for preschool children12, whilst the non-epidemic infection rate for Men B in Europe over 2014-16 was 10.5/100,000 in infants, 2.5/100,000 for 1-4 year olds, 0.8/100,000 for 5-24 year olds and 0.2-0.3 in older age groups13. Gender does not appear to be a factor, with infection rates being similar for boys and girls.
A comprehensive epidemiological review of IMD in Malta14 has confirmed an overall incidence rate for all types of meningococcal disease in 2000-2012 of 1.7/100,000, well above the European average of 1.1/100,000 for the same time period. The individual incidence rate was 0.99 and 0.3/100,000 for groups B and C, respectively, and the case fatality rate was above the European average, particularly with regard to Men C with 21% of cases compared with 11-15% for the rest of Europe14. Indeed, these figures would convincingly support the case for nationwide, population-based protection against Men C disease, particularly since several effective Men C vaccines have been widely available for almost two decades15. In contrast, this has not been the case for Men B where effective vaccine development has proven to be very difficult.
Early Men B vaccines
Early vaccines against Men C were purely polysaccharide-based and were designed to generate immunity against the meningococcal capsular polysaccharides. These vaccines were poorly immunogenic especially in those under the age of two, and had no effect on nasal carriage with waning protection over time16.
Protein-polysaccharide conjugate vaccines were later developed. These were found to be safe and effective, even in infants, against Men A, C and in combination e.g. ACWY. Further development of these vaccines with, for example, alterations in the adjuvant or type of carrier protein used, improved the vaccines immunogenicity17, and these conferred effective long term immunity. Consequently, over the past 15 years or so, many Men C/ACWY combination vaccines have been introduced into routine national schedules with very good effect. In the UK, nationwide Men C immunisation commenced in November 1999 and has reduced the rates of Men C disease in children to almost no cases per year18.
The situation with Men B was different. Unlike other meningococcal capsular groups, the Men B organism contains polysialic acid within its outer capsule, a compound that also forms part of the neural cell adhesion molecule (NCAM) in humans. This homophilic binding glycoprotein is expressed on several human cells including neurones, glia and skeletal muscle. Hence, its introduction within classical protein-polysaccharide conjugate vaccines derived from meningococcal B capsular components ensures that the vaccine is recognised as a ‘self-antigen’ and immune-tolerance guarantees a poor antibody response. An alternative approach was to revert to ‘whole cell’ vaccines but Men B strains are widely diverse and, therefore, several whole cell vaccines would be required to cover all major Men B pathogens. Other vaccines utilising protein antigenic components from the outer membrane vesicles (OMV) that are shed by the meningococcus during replication were developed. However, since the OMVs are strain-specific, these vaccines are only effective against meningococcal strains sharing the same proteins found in the OMVs. In practice, they proved effective in isolated outbreaks involving single strains in Norway in 1990 with 57.2% protection19, Cuba in 1990 with 83% efficacy20, and Normandy, France in 200321. In effect, these were tailor-made vaccines for isolated outbreaks and an alternative approach was required in order to design a vaccine that would offer effective protection for global endemic disease.
A new approach to vaccination
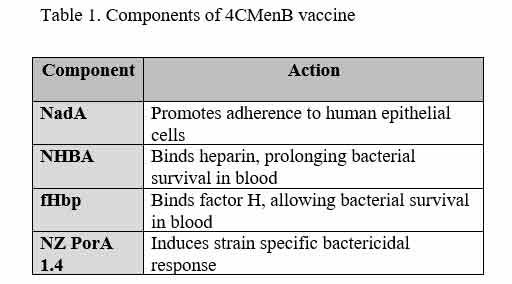
Reverse vaccinology was the phrase coined to describe this new approach. Using modern gene sequencing techniques, the entire meningococcus genome was determined, and repeatedly put through computer programmes to identify gene sequences that coded for antigenic proteins that, in turn, resulted in an immune response. To be ‘eligible’ for possible inclusion into a vaccine, these genes also had to be common to different meningococcal strains. Thousands of candidate genes were whittled down to just three major antigenic proteins (Table 1), and these were then combined with the OMV protein antigen from the strain-specific OMV vaccine developed in New Zealand in 1997, to create a new Men B vaccine22.
Early results of new vaccine
The resulting four-component Men B (4CMenB) vaccine was, during subsequent clinical trials, found to be safe and highly immunogenic against several strains of Men B23. A three dose priming course in the first few months (2, 4 and 6 months) followed by a booster dose at twelve months was shown to produce very high and persistent bactericidal antibody levels against all four components at 13 months24. This vaccine is based entirely on subcapsular meningococcal components and can, therefore, potentially offer some cross protection against other meningococcal serotypes that share these core proteins. Variations within Men B strains will account for some differences in immune response after vaccination, but a comprehensive review of Men B strains by country have predicted adequate cover against 80% of all currently circulating isolates (ranging from 66% in Canada to 91% in the USA, Figure 2)9.
To-date there have been no major safety issues, with around 25% of vaccinees developing a fever. This doubles to 50% if 4CMenB is given in combination with other vaccines and, for this reason, it has been recommended to co-administer paracetamol prophylactically together with the vaccine. This reduces the risk of fever to ‘background’ levels whilst also alleviating pain, fussiness and other minor adverse events25. Concerns have been raised that co-administering paracetamol reduces the immunogenicity of 4CMenB vaccines. However, although antibody responses to the 4CMenB vaccines are reduced with paracetamol, titres are still maintained well above seroprotective levels26.
Future considerations for 4CMenB
The difficulty, duration and complexity of developing this new vaccine have resulted in a hefty price tag (estimated at approximately €100 per dose, for a 3 or 4-dose programme). Given that meningococcal B is a rare disease affecting roughly 1:100,000 and has a varying incidence with fluctuating peaks and troughs over several-year cycles, the price for national vaccine coverage may be difficult to justify. Furthermore, there may be problems introducing yet another multi-dose vaccine into busy national immunisation schedules. On the other hand, this is offset by the severity of this disease with 10% mortality and 20% significant morbidity, and effectiveness of the vaccine. Indeed, the introduction of 4CMenB in Quebec, a highly endemic Men B region in Canada in 2013, and to selected university students in the US, resulted in no MenB cases and no safety issues in vaccinees27. Every country will need to weigh all options on an individual basis and, for example, the UK have altered their position from “not cost effective” in 2013 to “recommended for national coverage” by 2014 and introduced in 2015. Uptake for the first and second doses in the UK have now reached >95% and >90% of the target population, respectively, and within 10 months of introducing 4CMenB, the number of cases with Men B meningitis and/or septicaemia have halved. Other countries like France have introduced 4cMenB at a local level with encouraging preliminary results28.
Clearly, the results of post-immunisation surveillance from all these programmes will be awaited with great interest. Once wide coverage is attained and herd immunity established, it may well be possible to reduce the number of priming and booster doses required, as happened with Men C and Men ACWY vaccine programmes29.
Conclusion
To-date, the 4CMenB vaccine is the first effective preventative measure against this devastating disease. Although costly, it appears to be safe, and can be given with other vaccines although co-administered paracetamol is recommended. Long term surveillance to exclude any late adverse events and to determine the effectiveness and duration of protection is required. Individual countries will need to complete an individual country-specific exercise to establish the cost-benefit and feasibility of a 4CMenB programme.
References
- ECDC. Epidemiology of invasive meningococcal disease in Europe, 2008-2009. http://ecdc.europa.eu/en/healthtopics/vaccine-preventable-diseases/EU_IBD/laboratory_activities/Documents/IMD_2008-2009_ESPID_PHC.pdf
- Jafri RZ, Ali A, Messonnier NE, Tevi-Benissan C, Durrheim D, Eskola J, et al. Global epidemiology of invasive meningococcal disease. Popul Health Metr. 2013; 11(1): 17-25.
- 3. Stroffolini T. Vaccination campaign against meningococcal disease in army recruits in Italy. Epidemiol Infect. 1990; 105(3): 579-583.
- 4. ECDC. Surveillance of invasive bacterial diseases in Europe, 2015; pg47.
- Stein-Zamir C, Shoob H, Sokolov I, Kunbar A, Abramson N, Zimmerman D. The clinical features and long-term sequelae of invasive meningococcal disease in children. Pediatr Infect Dis J. 2014 Jul; 33(7):777-9.
- Campbell H, Borrow R, Salisbury D, Miller E. Meningococcal C conjugate vaccine: The experience in England and Wales. Vaccine. 2009; 27 (S2): B20-B29.
- Meningococcal meningitis. WHO 2015; update No.114. http://www.who.int/mediacentre/factsheets/fs141/en/
- Nadel S. Prospects for eradication of meningococcal disease. Arch Dis Child. 2012; 97: 993-998.
- Vogel U, Taha MK, Vazquez JA, Findlow J, Claus H, Stefanelli P, et al. Predicted strain coverage of a meningococcal multicomponent vaccine (4CMenB) in Europe: a qualitative and quantitative assessment. Lancet Infect Dis. 2013; 13 (5): 416-25.
- ECDC. Surveillance of invasive bacterial diseases in Europe, 2012; pg46.
- ECDC. Surveillance of invasive bacterial diseases in Europe, 2012; pg48.
- 12. Baker MG, Martin DR, Kieft CEM, Lennon D. A 10-year serogroup B meningococcal disease epidemic in New Zealand: Descriptive epidemiology, 1991–2000. J Pediatr Child Health. 2001; 37(s5): 13-19.
- ECDC. Surveillance atlas, Meningococcal disease in Europe, 2016.
- Pace D. Epidemiology of IMD in Malta. In Vaccine prevention of capsular group C meningococcal disease in children. PhD thesis 2016; ch5.
- Trotter CL, Andrews NJ, Kaczmarski EB, Miller E, Ramsay ME. Effectiveness of meningococcal serogroup C conjugate vaccine 4 years after introduction. Lancet. 2004 Jul 24-30; 364(9431): 365-7.
- Shea MW. The long road to an effective vaccine for meningococcus Group B (Men B). Ann Med Surg. 2013; 2(2): 53-56.
- Pace D, Snape M, Westcar S, Hamaluba M, Yu LM, Begg N, et al. A new combination Haemophilus influenzae type B and Neisseria meningitidis serogroup C-tetanus toxoid conjugate vaccine for primary immunization of infants. Pediatr Infect Dis J. 2007 Nov; 26(11): 1057-9.
- Success of Men C vaccination: Changes to the vaccination programme. Men C flyer for parents. NHS, UK. https://www.gov.uk/government/uploads/system/uploads/attachment_data/file/525375/MenC_flyer_for_parents_to_explain_the_schedule_change_May16.pdf
- Bjune G, Hoiby EA, Gronnesby JK, Arnesen O, Fredriksen JH, et al. Effect of outer membrane vesicle vaccine against group B meningococcal disease in Norway. Lancet. 1991; 338: 1093-96.
- Serra GV, Campa HC, Varcacel NM, et al. Vaccine against group B Neisseria meningitides: protection trial and mass vaccination in Cuba. NIPH Ann. 1991; 14 (2): 195-207.
- Delbos V, Lemée L, Bénichou J, Berthelot G, Deghmane AE, Leroy JP, et al. Impact of MenBvac, an outer membrane vesicle (OMV) vaccine, on the meningococcal carriage. Vaccine. 2013; 31: 4416-4420.
- Guiliani MM, Adu-Bobie J, Comanducci M, Aricò B, Savino S, Santini L, et al. A universal vaccine for serogroup B meningococcus. Proc Natl Acad Sci USA. 2006; 103 (29): 10834-39.
- 23. Mameli C, Galli E, Mantegazza C, Fabiano V, Zuccotti GV. The multicomponent meningococcal serogroup B vaccine (4CMenB): origin, composition, health impact and unknown aspects. Future Microbiol. 2015; 10(10): 1579-98.
- Vesikari T, Esposito S, Prymula R, Ypma E, Kohl I, Toneatto D, et al. Immunogenicity and safety of an investigational multicomponent, recombinant, meningococcal serogroup B vaccine (4CMenB) administered concomitantly with routine infant and child vaccinations: results of two randomised trials. Lancet. 2013; 381: 825-35.
- Prymula R, Esposito S, Zuccotti GV, Xie F, Toneatto D, Kohl I, Dull PM. A phase 2 randomized controlled trial of a multicomponent meningococcal serogroup B vaccine (I). Hum Vaccine Immunother. 2014; 10(7): 1993-2004.
- Das RR, Panigrahi I, Naik SS. The Effect of prophylactic antipyretic administration on post-vaccination adverse reactions and antibody response in children: A systematic review. Plos One. 2014; 9: e106629.
- Basta NE, Mahmoud AAF, Wolfson J, Ploss A, Heller BL, Hanna S, et al. Immunogenicity of a Meningococcal B Vaccine during a University Outbreak. NEJM, 2016; 375: 220-28.
- Levy C, Bechet S, Cohen R. Implementation of meningococcal B vaccination (Bexsero®) in France: Physicians’ perceptions and experiences of a few months after marketing approval. Arch Pediatr. 2016; 23(1): 27-33.
- Pace D, Khatami A, McKenna J, Campbell D, Attard-Montalto S, Birks J, et al. Immunogenicity of reduced dose priming schedules of serogroup C meningococcal conjugate vaccine followed by booster at 12 months in infants: open label randomised controlled trial. BMJ. 2015 Apr 1;350:h1554.
Acknowledgement
I would like to thank Dr David Pace for reviewing the manuscript.




