Peripheral arterial disease – a terrible misnomer
by Kevin Cassar MD(Malta) MMEd(Dundee) FRCS(Edin) MD(Aberdeen) FRCS(Intercoll)
Consultant Vascular Surgeon, Mater Dei Hospital
Peripheral arterial disease (PAD) has for far too long been treated as a minor ‘peripheral’ condition. The truth of the matter is that ‘peripheral’ arterial disease is associated with a three to four fold increased mortality compared to the general population. PAD is also associated with significantly increased morbidity from cardiovascular events such as myocardial infarction, cerebrovascular accidents and limb loss. Failure to recognise and treat risk factors in this group of patients results in preventable and unnecessary deaths, myocardial infarctions and strokes.
Introduction
Peripheral arterial disease (PAD) is cursed by its own name. The Oxford English Dictionary gives the meaning of the word ‘peripheral’ as “irrelevant, marginal, nonessential and unimportant”. Nothing could be further from the truth. PAD is only one manifestation of atherosclerosis, a systemic inflammatory condition affecting the coronary, cerebral and peripheral arteries. It is disease in the coronary and cerebral arterial beds that leads to the high mortality as well as the significant number of vascular events in this group of patients. There is abundant evidence to show that control of the major risk factors (hypertension, diabetes mellitus, hypercholesterolemia, cigarette smoking) and the administration of antiplatelet drugs can significantly reduce morbidity and mortality. Several national and international guidelines have been published to encourage adequate control of risk factors in an attempt to prevent deaths and vascular events. Despite these efforts, control of risk factors in this group of patients is often well below acceptable levels.
Peripheral arterial disease: just one manifestation of atherosclerosis
PAD, coronary artery disease and cerebral artery disease are all manifestations of the same systemic condition, atherosclerosis and it is therefore not surprising that the three conditions often affect the same patient. It is estimated that 65% of patients with PAD have coronary artery disease and/or cerebral artery disease.1 In the primary care setting, 50% of patients with PAD are found to have coronary artery disease or cerebral artery disease. In patients with PAD referred to hospital, the prevalence of coronary artery disease is even higher. Furthermore the extent of coronary artery disease increases with the severity of peripheral arterial disease as estimated by ankle brachial pressure index (ABPI).2 50% of patients with intermittent claudication are also found to have significant carotid disease on duplex ultrasonography.2
Prevalence and Incidence of PAD in Malta
PAD may be completely asymptomatic, may present with intermittent claudication of the calves, thighs and or buttocks, or in its most severe form may result in critical ischaemia defined as either ischaemic rest pain or ischaemic tissue loss (ulcers or gangrene).
PAD is a common condition. No epidemiological studies have been carried out in Malta to identify the prevalence of PAD. The overall annual incidence of intermittent claudication is estimated to be between 4.1-12.9 per 1000 in men and 3.3-8.2 per 1000 in women.3 Extrapolating this to our own population, we would expect an annual incidence of between 1333 and 5212 new patients with intermittent claudication based on a population of 404,039 (Census 2005 figures). Compare this to the incidence of all cancers (except squamous cell and basal cell carcinoma) reported for 2003 in Malta which was 659 (National Cancer Registry 2005).
The prevalence of PAD, based on an ABPI <0.9, ranges from 139-169 per 1000 in men and 114-205 per 1000 women over 55 years of age.4,5 Based on Census 2005 figures, the prevalence of PAD in Malta would be estimated to be between 15,652 and 28,147. These are huge numbers considering the size of our country and the resources available. Furthermore in view of the high prevalence of diabetes mellitus in Malta, it is likely that the true prevalence of PAD is likely to be towards the upper end of this estimate.
Morbidity and Mortality associated with PAD
The worse the severity of PAD as estimated by ABPI, the higher the risk of cardiovascular events and mortality. Death in this group of patients is overwhelmingly due to cardiovascular events with coronary artery disease accounting for 40-60%, cerebral artery disease for 10-20%, and ruptured abdominal aortic aneurysm accounting for another 10% of deaths.
In patients who have asymptomatic PAD or have intermittent claudication, the mildest form of the condition, the annual incidence of major cardiovascular events is between 5 and 7%.2 Taking the lowest estimate of PAD prevalence and assuming that all patients with PAD in Malta have the mildest form of disease, this would amount to around 1100 major cardiovascular events per year.
The outcomes in patients with critical limb ischaemia, the most severe end of the spectrum of PAD, are significantly worse. Patients with critical limb ischaemia have a mortality rate of 20% in the first year after presentation. Figure 2 summarises the results of several studies on mortality rates in patients with intermittent claudication and critical ischaemia compared to healthy controls. The striking point is that the 5 year mortality in patients with critical limb ischaemia is over 50%, worse than breast, colorectal or uterine cancer and similar to mortality from ovarian cancer (based on mortality data from the National Cancer Registry 2005).
Control risk factors and save lives
Controlling risk factors significantly reduces the high rate of morbidity and mortality in PAD. Current international guidelines2,6 recommend that all peripheral arterial disease patients should:
- Be prescribed an antiplatelet drug;
- Be prescribed a statin (unless their total serum cholesterol is below 3.5mmol/L);
- Stop smoking and be given help with smoking cessation (nicotine replacement treatment, bupropion, advice);
- Have their blood pressure controlled to less than 140/90mmHg or in diabetics or patients with renal insufficiency to less than 130/80mmHg;
- Have their blood glucose strictly controlled to achieve an HbA1c as close to 6% as possible if diabetic.
The use of antiplatelet drugs significantly reduces non-fatal myocardial infarction, non-fatal stroke and vascular death by a staggering 20%.7 Based on estimates of prevalence of PAD in Malta, prescribing antiplatelet drugs to all PAD patients would prevent between 253 and 456 vascular events (non-fatal MI, non-fatal stroke and vascular death) each year. The first line treatment should be 75mg Aspirin because of its low cost. The CAPRIE study however showed that 75mg clopidogrel daily is significantly more effective than aspirin at reducing myocardial infarction, stroke and death (relative risk reduction 24% compared to aspirin).8 In those who have contraindications to use of aspirin, clopidogrel is clearly an even more effective if somewhat more expensive treatment.
The Heart Protection Study showed that even patients with ‘normal’ cholesterol levels still had a marked benefit from statin use.9 Indeed the use of statins is associated with a 12% relative risk reduction in overall mortality, 17% reduction in vascular mortality, 24% reduction in coronary heart disease events, and a 27% reduction in all strokes.7 Extrapolating these figures to our local population, the use of statins would prevent between 281 and 506 deaths per year. Furthermore it would prevent between 313 and 562 cardiovascular events per year, besides cutting the number of strokes and the number of patients requiring coronary or peripheral revascularisation. Considering all of this and the documented cost-effectiveness of these treatments it seems rather short-sighted to decline this group of patients free drug treatment, as is the case currently. Unfortunately despite the high morbidity and mortality associated with this condition, peripheral arterial disease does not feature on the Schedule V list of conditions.
How well are we doing at controlling risk factors?
We recently presented the data from an audit on risk factor management in peripheral arterial disease carried out at St Luke’s Hospital.10 Of all patients with PAD referred to a vascular surgeon, only 43% were on an antiplatelet drug, only 17% were on a statin and only 10% had been given any help with smoking cessation. This compares very poorly with a similar audit carried out in Scotland where 72% of patients were on antiplatelet treatment, 85% were on a statin and 85% had been given help with smoking cessation.11 The major difference between these two countries is that all statins and antiplatelet drugs (including clopidogrel) are dispensed free of charge to Scottish patients and general practitioners are rewarded financially for achieving set targets.
The way forward
The prevalence of peripheral arterial disease will inevitably increase as the population grows older. It is high time that peripheral arterial disease sheds its “Cinderella” status. As clinicians we need to recognise the fact that this is a killer disease but more importantly that we can do something about it. Due pressure needs to be applied to the relevant health authorities to ensure that this group of patients are treated in the same way as patients with coronary heart disease with whom they share a common pathology, atherosclerosis, and equally high risks. Peripheral arterial disease patients deserve to be provided with the treatment required to reduce mortality and morbidity. Unless we act, we will continue to witness significant numbers of unnecessary and preventable deaths.
References
1.Bhatt D, Steg P, Ohman E et al. International prevalence, recognition and treatment of cardiovascular risk factors in outpatients with atherothrombosis. JAMA 2006; 295:180-9.
2.Norgren L, Hyatt WR, Dormandy JA et al. Intersociety consensus on the management of peripheral arterial disease. J Vasc Surg 2007; 45(1):S5A-S67A.
3.Meijer WT, Cost B, Bernsen RM et al. Incidence and management of intermittent claudication in primary care in the Netherlands. Scan J Primary Health Care 2002; 20:33-4.
4.Newman A, Siscovick DS, Manolio TA et al. Ankle-arm index as a marker of atherosclerosis in the Cardiovascular health study. Circulation 1993; 88:837-45.
5. Meijer WT, Hoes AW, Rutger D et al. Peripheral arterial disease in the elderly. The Rotterdam study. Arterioscler Thromb Vasc Biol 1998; 18:185-92.
6.SIGN guidelines Diagnosis and management of peripheral arterial disease. 2006. Available from: www.sign.ac.uk
7.Cassar K. Bachoo P. Peripheral arterial disease. Clin Evid 2006; (15):164-76.
8.CAPRIE steering committee. A randomised, blinded, trial of clopidogrel versus aspirin in patients at risk of ischaemic events (CAPRIE). Lancet 1996; 348(9038):1329-39.
9.Heart Protection Study Collaborative Group. MRC/BHF Heart Protection Study of cholesterol lowering with simvastatin in 20,536 high-risk individuals: a randomised placebo-controlled trial. Lancet 2002; 360(9326):7-22.
10. Mercieca A, Cassar K. Are international guidelines being applied in peripheral arterial disease? Paper presented at “Taking Primary Health Care in Malta to New Heights” Primary Health Care Department Biannual Conference, Malta[e1] .
11. Cassar K, Coull R, Bachoo P, Macaulay E, Brittenden J. Management of secondary risk factors in patients with intermittent claudication. Eur J Vasc Endovasc Surg 2003; 26:262-6.
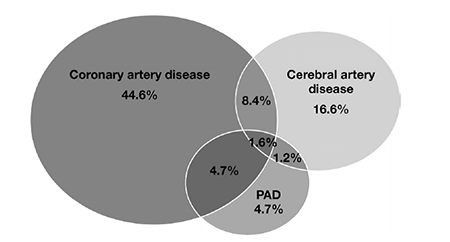
Figure 1: Degree of overlap between the three conditions
(Source: Norgren L, Hyatt WR, Dormandy JA et al. Intersociety consensus on the management of peripheral arterial disease)
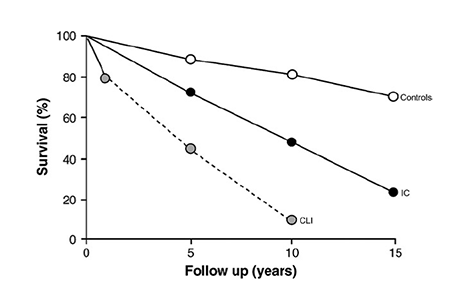
Figure 2: Survival rate for controls, IC (Intermittent claudication) and CLI (critical limb ischaemia)
(Source: Norgren L, Hyatt WR, Dormandy JA et al. Intersociety consensus on the management of peripheral arterial disease)

